How Drug Shortages Are Putting Patient Care at Risk
 Nov, 20 2025
Nov, 20 2025
When a patient needs a life-saving drug and it’s simply not available, the consequences aren’t theoretical-they’re immediate. A child with leukemia waits weeks for asparaginase. A cardiac patient gets a less reliable anticoagulant because heparin is gone. An elderly person with severe pain skips doses because their opioid prescription can’t be filled. These aren’t rare exceptions. They’re everyday realities in U.S. hospitals right now.
What’s Really Going On With Drug Shortages?
Drug shortages aren’t new, but they’ve reached a breaking point. As of June 2025, there were still 253 active drug shortages in the U.S., according to the American Society of Health-System Pharmacists (ASHP). That’s down from a peak of 323 in early 2024, but still far higher than the 187 shortages recorded in 2021. Most of these shortages started after 2022, meaning this isn’t a lingering problem-it’s accelerating. The majority of these shortages involve generic drugs, which make up 83% of the list. Why? Because manufacturers have little financial incentive to produce low-margin medications. A single vial of a generic antibiotic might cost $2. A company that spends millions to upgrade a factory for quality compliance won’t make back that investment on a drug that sells for pennies. So they shut down production, and the supply vanishes. The root causes are structural: 47% of shortages come from fractured global supply chains, 32% from manufacturing quality failures, and 21% from raw material shortages. A single factory in India or China that fails an FDA inspection can wipe out the entire U.S. supply of a critical drug. And there’s no backup.How Shortages Directly Hurt Patients
It’s not just about inconvenience. When a drug disappears, patients suffer. In oncology, delays of 7 to 14 days during asparaginase shortages have been linked to lower survival rates in children with acute lymphoblastic leukemia. For patients with rare cancers, there are often no alternatives. Nelarabine, used for T-cell leukemia, has been in shortage for over four years. Doctors are forced to use older, more toxic drugs-or worse, delay treatment entirely. In emergency and surgical care, heparin shortages have forced cardiac centers to switch to alternative anticoagulants. This isn’t a simple swap. These alternatives require different dosing, more monitoring, and longer procedures-increasing surgery time by 22%. That means more time under anesthesia, higher risk of complications, and longer hospital stays. Even common medications are affected. Lorazepam injections, used for seizures and severe anxiety, are often unavailable. Patients with epilepsy risk breakthrough seizures. Those in emergency rooms face longer waits while staff scramble to find a substitute. A 2024 JAMA Network Open study found that nearly one in three patients either skipped doses, took less than prescribed, or didn’t fill prescriptions at all because of shortages or cost. That’s not adherence-it’s survival strategy.The Hidden Burden on Healthcare Workers
Behind every shortage is a team of pharmacists, nurses, and doctors working overtime to keep patients safe. Hospitals now monitor an average of 43 drug shortages at once. For pediatric units, that number jumps to 54. Each shortage demands 15 to 20 hours of staff time per week-just to find alternatives, update protocols, train staff, and communicate changes. Pediatric facilities need 25% more time because children’s doses are more complex and fewer alternatives exist. One hospital pharmacist described it like playing 10 simultaneous games of chess while the board keeps changing. One day, it’s IV saline bags. The next, it’s insulin. Then antibiotics. Then sedatives. Each switch carries risk. Medication errors linked to shortages jumped 43% between 2019 and 2024. That’s not a typo. It’s a crisis. Nurses are forced to use unfamiliar drugs they haven’t been trained on. Pharmacists spend hours calling distributors, checking inventory across states, and begging for small quantities. In some cases, they’ve had to split single vials among multiple patients to stretch supply.
Costs That Go Beyond the Price Tag
Drug shortages cost the U.S. healthcare system nearly $900 million a year in extra labor alone. That doesn’t include the cost of more expensive alternative drugs, cancelled surgeries, longer hospital stays, or emergency room visits caused by untreated conditions. Patients pay too. Out-of-pocket costs rise by an average of 18.7% during shortages because alternatives are often newer, branded, or off-label drugs with no generic competition. One study found that 31% of pharmacy directors reported adverse events directly tied to shortages-including overdoses from incorrect substitutions, allergic reactions, and treatment failures. And it’s not just hospitals. Outpatient infusion centers-where patients receive chemotherapy, immunotherapy, or IV antibiotics-have seen 41% of treatments delayed, omitted, or rescheduled. For cancer patients, that’s not just a scheduling issue. It’s a threat to survival.What’s Being Done-And Why It’s Not Enough
There are efforts to fix this. The FDA’s Drug Shortage Electronic Registration and Notification Act, which took effect in January 2023, requires manufacturers to report potential shortages six months in advance. That’s a step forward. But many shortages still come out of nowhere. Some hospitals have formed shortage management committees. Others use real-time monitoring tools from group purchasing organizations like Vizient. These tools have saved hospitals $300 million in avoided inventory costs since 2023. But they don’t solve the root problem: no one is forcing drugmakers to keep producing low-profit medications. Congress held hearings in late 2023 and early 2024. The Biden administration included drug supply chains in its 2022 Executive Order on America’s Supply Chains. But there’s been no major policy shift-no subsidies, no guaranteed minimum production quotas, no penalties for companies that abandon critical drugs. The result? A system that’s constantly firefighting, never preventing.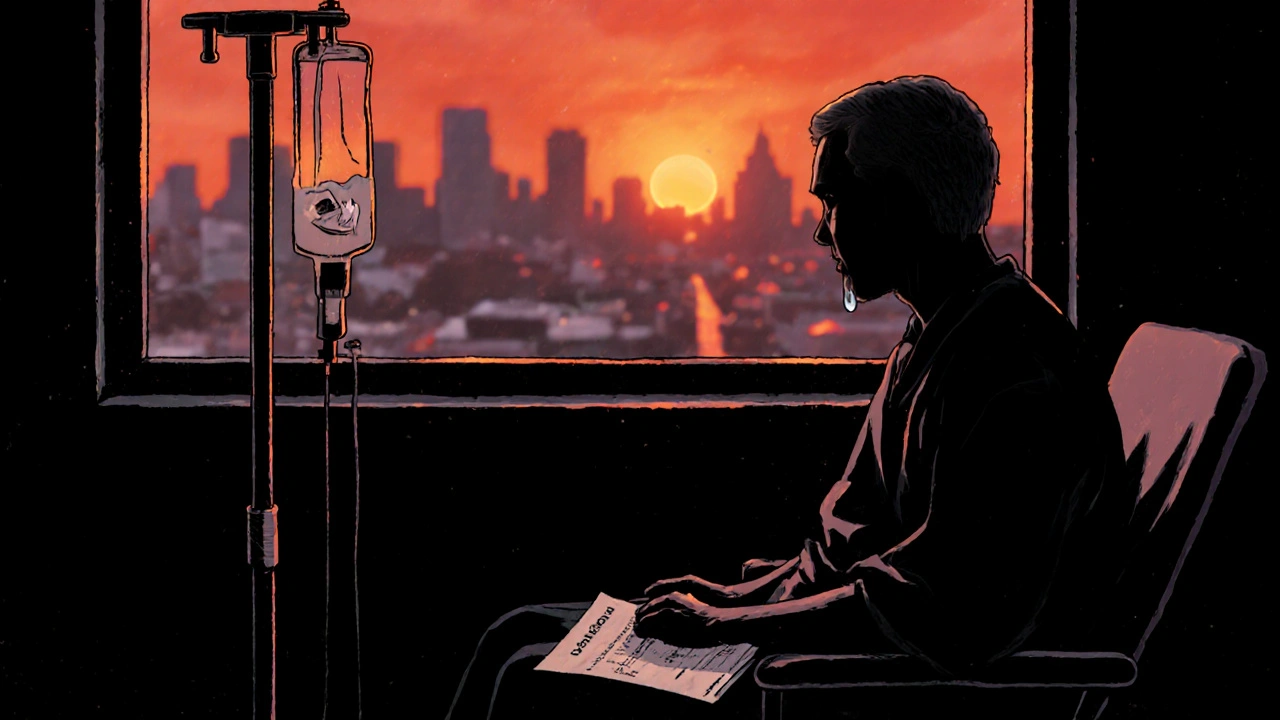
What This Means for You
If you or a loved one relies on a chronic medication-whether it’s for diabetes, heart disease, epilepsy, or cancer-you need to be prepared. Talk to your pharmacist. Ask if your medication is on the shortage list. Ask what alternatives exist and whether they’re safe for you. Ask if your doctor can prescribe a different formulation or brand. Don’t assume your prescription will be filled. Keep a 7- to 10-day backup supply if possible. If you’re on a long-term treatment, consider switching to a different pharmacy or provider who may have better access. And speak up. If you’ve had to skip doses, delay treatment, or pay more because of a shortage, tell your doctor. Share your story. The only way this system changes is when patients demand it.Where Do We Go From Here?
This isn’t just a pharmacy problem. It’s a public health emergency. We can’t keep patching a broken system with workarounds. We need policies that reward manufacturers for producing essential generic drugs-not just the profitable ones. We need stockpiles of critical medications, like we have for vaccines and pandemic supplies. We need transparency so hospitals know weeks ahead when a drug is at risk. Until then, the burden falls on patients and frontline workers. And every day, someone is forced to choose between a treatment that might not work and no treatment at all. The drugs are supposed to save lives. Right now, the system is making them harder to get.Why are generic drugs more likely to be in shortage?
Generic drugs make up 83% of current shortages because they’re low-margin products. Manufacturers earn very little per pill or vial, so when production costs rise-due to FDA inspections, raw material shortages, or labor issues-they often shut down production rather than absorb the loss. There’s little financial incentive to keep making these essential but inexpensive medications.
Can drug shortages cause medical errors?
Yes. Medication errors directly linked to drug shortages increased by 43% between 2019 and 2024. When pharmacists and nurses have to switch to unfamiliar alternatives, dosing mistakes, allergic reactions, and incorrect administration become more common. Studies show error rates spike by 18.3% during transitions to substitute drugs.
Are there any drugs that have been in shortage for years?
Yes. Drugs like asparaginase (used for childhood leukemia), nelarabine (for T-cell leukemia), and heparin (an anticoagulant) have been in shortage for three to five years. These aren’t temporary glitches-they’re systemic failures. For some patients, there are no safe or effective alternatives.
How do shortages affect children differently?
Children are hit harder because many drugs don’t come in pediatric-friendly forms. A drug available as a tablet for adults might only come in a vial for IV use in kids. When those vials are in short supply, there are often no alternatives. Pediatric facilities spend 25% more staff time managing shortages than general hospitals because of this complexity.
What can patients do if their medication is unavailable?
First, talk to your pharmacist and doctor. Ask if there’s a safe alternative or if you can switch brands. Keep a small backup supply if possible. Don’t skip doses without medical advice. If you’re struggling to get your medication, report it to your provider and consider contacting patient advocacy groups. Your experience helps highlight the scale of the problem.
Matthew Mahar
November 22, 2025 AT 17:22This is insane. I had to watch my cousin’s kid go through chemo with half the dose because asparaginase was gone. No one talks about how it feels to sit in a hospital room and hear the nurse say, ‘We’re trying to find it.’ Like, what do you mean ‘trying’? It’s a life-saving drug. Not a limited-edition sneaker.
Pramod Kumar
November 23, 2025 AT 19:17Man, I work in a pharmacy in Delhi, and we see this all the time with antibiotics and insulin. But here’s the twist-we don’t have the luxury of alternatives. In the U.S., you at least have ten different options, even if they’re expensive. In India, if it’s gone, it’s gone. No backup, no bureaucracy, no lobbying. Just silence and suffering. We need global supply chains that don’t treat life-saving meds like commodities.
Richard Wöhrl
November 25, 2025 AT 05:46Let me just say this: the 43% increase in medication errors since 2019? That’s not a statistic-that’s a body count. I’ve seen nurses give insulin doses based on memory because the label was wrong, and the vial they grabbed wasn’t the one they were supposed to. And it’s not negligence-it’s exhaustion. They’re not trained for this. No one trains you to be a drug shortage detective. The system is failing them. And we’re letting it.
shreyas yashas
November 25, 2025 AT 11:57My uncle’s on warfarin. They switched him to apixaban because heparin was out. He bled internally. Turned out the dose was wrong. Took three weeks to stabilize. No one warned us. No one told us the alternatives were riskier. This isn’t a ‘supply chain issue.’ It’s a moral failure. And we’re all just scrolling past it.
Suresh Ramaiyan
November 26, 2025 AT 01:27It’s funny how we build rockets to Mars but can’t guarantee a child gets their cancer drug. We optimize for profit in a system where profit shouldn’t be the metric. Maybe we need to treat essential drugs like public infrastructure-like water, like electricity. You don’t let a company decide whether your town gets clean water based on quarterly earnings. Why do we accept this with medicine?
Vivian C Martinez
November 27, 2025 AT 00:43You’re not alone. I’m a nurse in Ohio. We had to split one vial of lorazepam between three seizure patients last week. One of them was 8 years old. We weighed the dose on a milligram scale. We cried after. This isn’t healthcare. It’s triage with a clipboard.
Casper van Hoof
November 28, 2025 AT 06:51One might argue that the market, left to its own devices, will eventually correct this imbalance through innovation or consolidation. However, the empirical evidence suggests that the incentive structure is fundamentally misaligned with public health imperatives. The commodification of biological necessity has created a structural pathology that cannot be resolved by market mechanisms alone.
Adrian Rios
November 28, 2025 AT 22:18Let me tell you something that no one wants to admit: the FDA’s six-month notice rule? It’s a joke. I work in a hospital pharmacy. We get a notice about a shortage in January-and by February, the drug’s already gone. The manufacturers? They wait until the last possible second to file. Why? Because if they file early, they get tagged as ‘at risk’ and their stock drops. So they gamble with people’s lives. And the FDA? They just sit there with their clipboard and say, ‘We’re monitoring.’ That’s not oversight. That’s complicity.
Brandy Walley
November 30, 2025 AT 00:29John Mackaill
December 1, 2025 AT 08:04Brandy, I get it-you think this is overblown. But let me ask you this: if your child needed a drug that vanished because a factory in China failed an inspection, and the only alternative had a 30% higher risk of organ damage, would you still say it’s ‘just fearmongering’? This isn’t politics. It’s biology. And biology doesn’t care about your ideology.