Statins and Antifungal Medications: How Their Interaction Can Cause Dangerous Muscle Damage
 Dec, 15 2025
Dec, 15 2025
Statin-Antifungal Interaction Checker
Check Your Medication Risk
Select your statin and antifungal to determine the risk level and what you should do.
Imagine taking a statin to lower your cholesterol and then getting a prescription for an antifungal cream or pill for a stubborn yeast infection. Sounds harmless, right? But if you’re on the wrong statin and the wrong antifungal, this common combo can trigger a life-threatening condition called rhabdomyolysis - where your muscles start breaking down, flooding your bloodstream with toxic proteins that can shut down your kidneys.
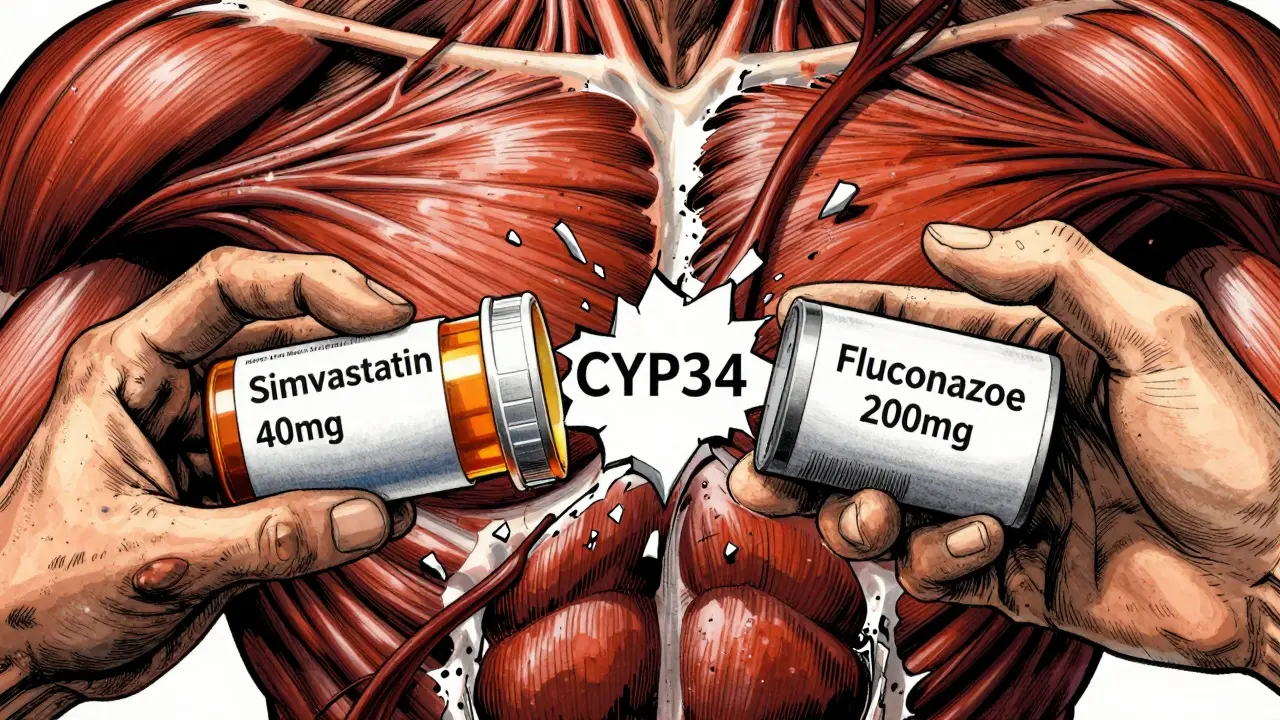
Why This Interaction Isn’t Just a Warning - It’s a Red Flag
Statins like simvastatin, lovastatin, and atorvastatin work by blocking an enzyme in your liver that makes cholesterol. But here’s the catch: your body uses a system called CYP3A4 to break down these drugs. Azole antifungals - including itraconazole, voriconazole, and even fluconazole - are powerful inhibitors of that same enzyme. When they’re taken together, your body can’t clear the statin fast enough. The statin builds up. And when it builds up too much, it starts attacking your muscle cells. This isn’t theoretical. In 2012, the FDA updated safety labels after reviewing dozens of cases where patients on simvastatin and itraconazole developed rhabdomyolysis. One study showed that combining simvastatin with itraconazole spiked simvastatin levels by over 1,000%. That’s not a small bump - it’s a tsunami.Not All Statins Are Created Equal
Some statins are far more dangerous when paired with antifungals. Here’s the breakdown:- High risk: Simvastatin, lovastatin - these are almost entirely broken down by CYP3A4. Even low doses can become toxic with antifungals.
- Medium risk: Atorvastatin - still metabolized by CYP3A4, but less sensitive. Still dangerous with strong inhibitors like itraconazole.
- Low risk: Pravastatin, fluvastatin, rosuvastatin, pitavastatin - these mostly avoid CYP3A4. They’re your safer options if you need an antifungal.
Let’s say you’re on 40 mg of simvastatin and your doctor prescribes fluconazole for a yeast infection. That’s not a green light. Fluconazole is a weaker CYP3A4 blocker than itraconazole, but at 200 mg or higher, it can still boost simvastatin levels by 350%. That’s enough to push you into danger territory.
What Rhabdomyolysis Actually Feels Like
This isn’t a sore muscle after a workout. This is something different - and terrifying.- Severe muscle pain, especially in your thighs, shoulders, or lower back - so bad you can’t stand up or lift your arms.
- Weakness so intense you can’t climb stairs or get out of a chair.
- Dark, tea-colored urine - a sign that muscle proteins are leaking into your blood and your kidneys are struggling to filter them.
One case from 2018 involved a 68-year-old man who took simvastatin 40 mg daily and fluconazole 200 mg for toenail fungus. Seven days later, his creatine kinase (CK) levels hit 18,400 U/L. Normal range? 30-200 U/L. He spent three days in the hospital. He didn’t die - but he could have.
On Reddit, pharmacists report seeing 2-3 cases a year from this exact combo. Most are elderly patients with other health problems. Many didn’t even know they were at risk.
The Real Culprits: Which Antifungals Are the Most Dangerous?
Not all antifungals are equal. Here’s how they stack up as CYP3A4 inhibitors:- Strongest: Ketoconazole, itraconazole - these are absolute no-gos with simvastatin or lovastatin. The FDA says: don’t mix them.
- Strong: Voriconazole - also high risk. Avoid with simvastatin, lovastatin, and even high-dose atorvastatin.
- Moderate: Fluconazole - especially at doses above 200 mg/day. Still risky with simvastatin. Safer with pravastatin or rosuvastatin.
- Lowest risk: Isavuconazole - a newer antifungal approved in 2015 that barely touches CYP3A4. A real game-changer for patients who need long-term treatment.
One 2023 study found that isavuconazole didn’t raise simvastatin levels at all. That’s huge. If you’re on long-term antifungals - say for a chronic fungal lung infection - ask your doctor about switching to isavuconazole.
What Doctors Should Do - And What You Should Ask
Your doctor doesn’t always know your full med list. That’s why you need to speak up.- If you’re on simvastatin or lovastatin: Tell your doctor you’re taking it before they prescribe ANY antifungal. Even an over-the-counter antifungal cream can be absorbed enough to cause problems.
- If you’re on atorvastatin: Ask if the antifungal is a strong CYP3A4 inhibitor. If it is, your dose may need to drop to 20 mg or less.
- Ask for alternatives: Can you switch to pravastatin or rosuvastatin? Both are just as effective for lowering cholesterol - and they’re safe with antifungals.
- Get a baseline CK test: If you must take a risky combo, your doctor should check your creatine kinase before you start and again after a week.
Hospitals have started building hard stops in their electronic systems. If you’re prescribed simvastatin 40 mg and itraconazole, the system blocks it. At Mayo Clinic, this cut dangerous prescriptions by 87%. But outside hospitals? In pharmacies and clinics? The system still fails - often.

What to Do If You’re Already on a Risky Combo
If you’re currently taking simvastatin or lovastatin with itraconazole, voriconazole, or high-dose fluconazole:- Don’t stop either drug cold. That can be dangerous too.
- Call your doctor or pharmacist immediately. Say: “I’m on [your statin] and [your antifungal]. I’ve heard this combo can cause muscle damage. What should I do?”
- Watch for symptoms: Muscle pain, weakness, dark urine - even mild versions. If you notice them, stop the statin and get checked right away.
- Ask about switching: Can you switch statins? Can you switch antifungals? Isavuconazole or topical antifungals might be safer.
What’s New - And What’s Coming
The good news? We’re getting smarter.- Genetic testing is starting to show that people with a CYP3A5*3/*3 gene variant (about 1 in 3 people of European descent) are more likely to build up statins - even at normal doses - when combined with antifungals.
- New guidelines from the American College of Cardiology and Infectious Diseases Society of America are coming in early 2024. They’ll give doctors step-by-step decision trees based on age, kidney function, and drug doses.
- Pharmacists are now trained to flag these combos at the pharmacy counter. If you’re picking up a statin and an antifungal, ask: “Is this combo safe?”
Between 2015 and 2022, rhabdomyolysis cases from this interaction dropped by 34%. That’s because more doctors know about it. More systems block it. More patients ask questions.
Bottom Line: You’re Not Overreacting
If you’re on a statin and need an antifungal, this isn’t something to brush off. It’s one of the most common preventable drug interactions that leads to hospitalization - and sometimes death. The risk isn’t small. The consequences aren’t minor.But here’s the hopeful part: it’s almost always avoidable. Switch your statin. Switch your antifungal. Or pause one until the other is done. You don’t have to choose between your heart and your skin. There’s a safe path - you just need to ask for it.
Can I take fluconazole with my statin?
It depends on which statin you’re on. Fluconazole is a moderate CYP3A4 inhibitor. If you’re taking simvastatin or lovastatin, it’s unsafe at doses above 200 mg/day. For atorvastatin, keep the dose at 20 mg or lower. If you’re on pravastatin, fluvastatin, rosuvastatin, or pitavastatin, fluconazole is generally safe at standard doses. Always check with your doctor or pharmacist before combining them.
Is rhabdomyolysis reversible?
Yes - if caught early. Stopping the drugs and getting fluids and monitoring can fully reverse muscle damage in most cases. But if kidney failure develops, it can lead to long-term dialysis or even death. That’s why early symptoms like muscle pain and dark urine are critical warning signs. Don’t wait.
What’s the safest statin to take with antifungals?
Pravastatin and rosuvastatin are the safest options. They’re not broken down by CYP3A4, so antifungals won’t cause them to build up. Fluvastatin is also low-risk. If you need long-term antifungal therapy, switching to one of these is often the best move - and it won’t hurt your cholesterol control.
Can I use antifungal cream instead of pills?
Topical antifungals (like clotrimazole or terbinafine cream) are much safer because very little enters your bloodstream. But even some topical azoles - especially if used over large areas or broken skin - can be absorbed enough to cause problems with high-risk statins. When in doubt, ask your pharmacist: “Is this cream safe with my statin?”
Why don’t doctors always catch this?
Many doctors don’t have time to check every drug interaction, especially in busy outpatient clinics. Patients often don’t mention OTC antifungals or supplements. Plus, some statins - like rosuvastatin - are safe, so the interaction isn’t obvious unless you know which one you’re on. That’s why it’s up to you to know your meds and speak up.
How long does the interaction last after stopping the antifungal?
CYP3A4 inhibition can last days after you stop the antifungal. For itraconazole or voriconazole, wait at least 3-7 days after finishing the course before restarting a high-risk statin. For fluconazole, 2-3 days is usually enough. Always confirm with your doctor - don’t guess.
Thomas Anderson
December 16, 2025 AT 07:03Just got prescribed fluconazole for a yeast infection and was about to panic-glad I checked this. I’m on rosuvastatin, so I’m good, but wow, this is wild. My grandma almost went to the ER last year from the same combo with simvastatin. Always ask your pharmacist.
Dwayne hiers
December 17, 2025 AT 08:54The CYP3A4-mediated pharmacokinetic interaction between azole antifungals and HMG-CoA reductase inhibitors is a well-documented clinical phenomenon. Simvastatin and lovastatin, being highly lipophilic and predominantly metabolized by CYP3A4, exhibit exponential increases in AUC and Cmax when co-administered with potent inhibitors like itraconazole. The 1000% increase in simvastatin exposure is not an outlier-it’s a predictable pharmacodynamic consequence of enzyme saturation. Pravastatin and rosuvastatin remain first-line alternatives due to their minimal CYP3A4 involvement and renal excretion pathways.
Furthermore, fluconazole’s dose-dependent inhibition necessitates caution even at 200 mg/day. Recent FDA guidance recommends dose reduction of atorvastatin to ≤20 mg when co-administered with moderate inhibitors. The 2023 isavuconazole data is promising, with negligible CYP3A4 inhibition and comparable efficacy in invasive fungal infections. Pharmacogenomic testing for CYP3A5*3 alleles may further stratify risk in populations of European descent.
Electronic health record alerts have demonstrably reduced adverse events, but community pharmacy systems remain inconsistent. Clinicians must proactively screen for OTC antifungal use, including topical azoles applied to large surface areas or compromised skin. CK monitoring pre- and post-initiation is non-negotiable in high-risk combinations.
Edward Stevens
December 18, 2025 AT 07:16So let me get this straight-we’ve got a billion-dollar pharmaceutical industry that sells us statins, then another billion-dollar industry selling us antifungals, and neither one of them bothers to tell us the combo might turn our muscles into soup? And we wonder why people don’t trust doctors.
Alexis Wright
December 18, 2025 AT 20:43They don’t want you to know this. The pharmaceutical-industrial complex profits from chronic disease, not cures. Statins keep you dependent. Antifungals? They’re just another hook. The FDA’s ‘updates’ are PR stunts. Real change? It comes from people like you waking up. And yet, you still take the pills. You still trust the system. You’re part of the problem. The real danger isn’t rhabdomyolysis-it’s your complacency. You’d rather die quietly than ask a hard question.
And don’t even get me started on ‘isavuconazole.’ It’s not a breakthrough-it’s a placebo with a fancy name. They’re just rebranding the same old poison with a new label. The CYP3A4 pathway isn’t broken-it’s being weaponized. They want you weak. They want you scared. They want you dependent. Wake up.
And if you think switching statins solves anything-you’re fooling yourself. The system doesn’t care if you live or die. It cares about quarterly earnings. This isn’t medicine. It’s a casino. And you’re the sucker holding the losing hand.
Don’t just ‘ask your doctor.’ Demand answers. Demand alternatives. Demand transparency. Or stop pretending you’re in control.
Daniel Wevik
December 18, 2025 AT 21:08This is exactly why medication reconciliation needs to be standard practice, not an afterthought. Every patient on chronic therapy-especially statins-should have a documented drug interaction profile reviewed at least annually. Pharmacists are the unsung heroes here. If you’re picking up a script, ask: ‘Is this safe with my other meds?’ Don’t wait for symptoms. Prevention is 100x easier than recovery.
And if you’re on simvastatin and your doctor prescribes fluconazole? Push back. Say: ‘I know this combo can be dangerous. Can we switch me to rosuvastatin?’ Most docs will agree-it’s not a hassle. It’s just better medicine.
Knowledge isn’t power. Action is. Don’t be passive. Be proactive. Your muscles will thank you.
Rich Robertson
December 19, 2025 AT 15:13My uncle in Texas had this happen. Took simvastatin for 8 years, then got a fungal nail infection. Used fluconazole 200 mg for a month. One morning he couldn’t lift his coffee cup. Dark urine. Hospital for a week. Never took statins again. Now he takes ezetimibe and walks 5 miles a day. Lives better than before.
It’s not just about the drugs. It’s about the system. Doctors are rushed. Pharmacies are understaffed. Patients are tired. But if you’re on meds long-term? You owe it to yourself to know how they interact. Not just the side effects-how they play with other stuff.
And yeah, topical antifungals aren’t always safe either. I used clotrimazole cream on my feet for months and didn’t think twice. Turns out, if you’ve got cracked skin and use it daily? You’re absorbing more than you think.
Bottom line: You’re the CEO of your body. Don’t outsource your safety.
Rulich Pretorius
December 21, 2025 AT 09:32In South Africa, we don’t always have access to the latest antifungals or the safest statins. Many patients are on simvastatin because it’s cheap. Fluconazole is everywhere-it’s used for thrush, for candida, even for suspected fungal infections without testing. The risk is real, but so is the lack of alternatives.
I’ve seen patients who couldn’t afford to switch statins, so they just stopped the antifungal early. That’s dangerous too. Fungal infections come back stronger. It’s a lose-lose.
What we need isn’t just awareness-it’s affordable access. Rosuvastatin is effective, but in rural clinics? It’s often not stocked. We need policies that prioritize safe, not just cheap. Because in the end, a hospital bill for rhabdomyolysis costs more than a better statin ever could.
Ask your doctor. Push for alternatives. But also, push for change beyond the individual level.
Jonny Moran
December 22, 2025 AT 09:52Just had a friend tell me her mom was hospitalized for this. She didn’t even know she was on simvastatin-thought it was just a ‘cholesterol pill.’ The pharmacist didn’t flag it. The doctor didn’t mention it. She took fluconazole for a yeast infection and woke up feeling like she’d been hit by a truck.
People need to know this. Not just the elderly. Younger people take statins now too. And antifungals? Everyone gets a fungal infection at some point. This isn’t rare. It’s silent. And it’s preventable.
If you’re on a statin and need an antifungal, don’t assume it’s fine. Don’t Google it and hope for the best. Talk to someone who knows. A pharmacist. A nurse. Someone who’s seen this before.
You’re not being paranoid. You’re being smart.
Sinéad Griffin
December 23, 2025 AT 00:12AMERICA NEEDS TO STOP LETTING BIG PHARMA GET AWAY WITH THIS 💀🩸
They sell you statins like candy, then when you get sick, they act like it’s YOUR FAULT for taking the antifungal. NO. IT’S THEIR FAULT FOR NOT LABELING IT CLEARLY. I’M SO MAD RIGHT NOW.
MY DAD HAD THIS. HE WAS 62. THEY SAID ‘IT’S JUST MUSCLE PAIN.’ TWO WEEKS LATER HE WAS ON DIALYSIS. DON’T LET THIS HAPPEN TO YOU.
SWITCH STATINS. ASK QUESTIONS. STAND UP. 🇺🇸✊
Daniel Thompson
December 24, 2025 AT 16:18I work in a hospital pharmacy. We have a hard stop in our system for simvastatin + itraconazole. It blocks the prescription. But we still get overrides. Sometimes the doctor clicks through it. Sometimes the patient insists. And sometimes, they’re right-but they shouldn’t have to be.
The real issue isn’t the interaction. It’s the lack of coordination between prescribers, pharmacists, and patients. We all have pieces of the puzzle. But no one has the whole picture.
If you’re on a statin, keep a list. Bring it to every appointment. Even if it’s just on your phone. Even if your doctor says they have it. Show it to them.
It’s not about distrust. It’s about clarity.
Natalie Koeber
December 25, 2025 AT 02:23you know what else they dont tell you? the statins are linked to the cia mind control program. the antifungals? they’re just masking the side effects so you dont notice you’re being programmed. dark urine? that’s the nanites reacting. your muscles breaking down? they’re harvesting your bio-energy for the new world order. the ‘isavuconazole’ they’re pushing? it’s a placebo designed to make you feel safe while they keep feeding you the real poison. don’t trust the ‘experts.’ they’re all in on it.
Wade Mercer
December 26, 2025 AT 20:58People who take statins are already making a choice to medicate a symptom instead of fixing the root cause. Poor diet. No exercise. Stress. And now you’re surprised when the drugs you took to ‘fix’ your cholesterol start destroying your muscles? This isn’t a drug interaction problem. This is a moral failure. You chose convenience over health. Now you’re mad because the consequences caught up?
Stop blaming the system. Start taking responsibility. Your body isn’t a machine you can tweak with pills. It’s a temple. And you’re desecrating it.
Sarthak Jain
December 28, 2025 AT 15:55Bro i was on atorvastatin 40mg and got fluconazole 150mg for jock itch… i felt so weak i couldnt even walk to the bathroom. i thought i was having a heart attack. turned out my ck was 8000. i switched to rosuvastatin and never looked back. also, i never knew topical antifungals could be risky-used terbinafine cream for months. my doc said its fine but now im paranoid lol. always ask. always double check. your life matters more than saving 5 mins.
Tim Bartik
December 29, 2025 AT 16:23Statins? More like ‘statin-stupid.’ You think your cholesterol’s the problem? Nah. It’s the sugar. It’s the processed crap you eat. You take a pill to cover up the fact you live on pizza and soda, then you get some antifungal cream for athlete’s foot and suddenly your legs turn to jelly? DUH. The real danger isn’t the drug combo-it’s the lifestyle that got you here in the first place.
And don’t even get me started on ‘safe’ statins. Rosuvastatin? That’s just the new fancy pill with a bigger price tag. Same damn thing. Just wrapped in a prettier bow.
Go eat real food. Walk more. Sleep. Stop treating your body like a broken toaster you keep duct-taping.
Dwayne hiers
December 31, 2025 AT 02:21Thank you for the detailed breakdown. I’d add one more nuance: CYP3A4 inhibition isn’t binary. Even ‘low-risk’ statins can be affected by prolonged, high-dose exposure to inhibitors-especially in elderly patients with reduced renal clearance. The 2024 ACC/IDSA guidelines will likely emphasize individualized risk stratification based on age, eGFR, and concomitant polypharmacy. For patients >75 or with CKD, even rosuvastatin may require dose adjustment in the presence of moderate inhibitors. Always err on the side of caution.