Spondylolisthesis: Understanding Back Pain, Instability, and Fusion Options
 Dec, 15 2025
Dec, 15 2025
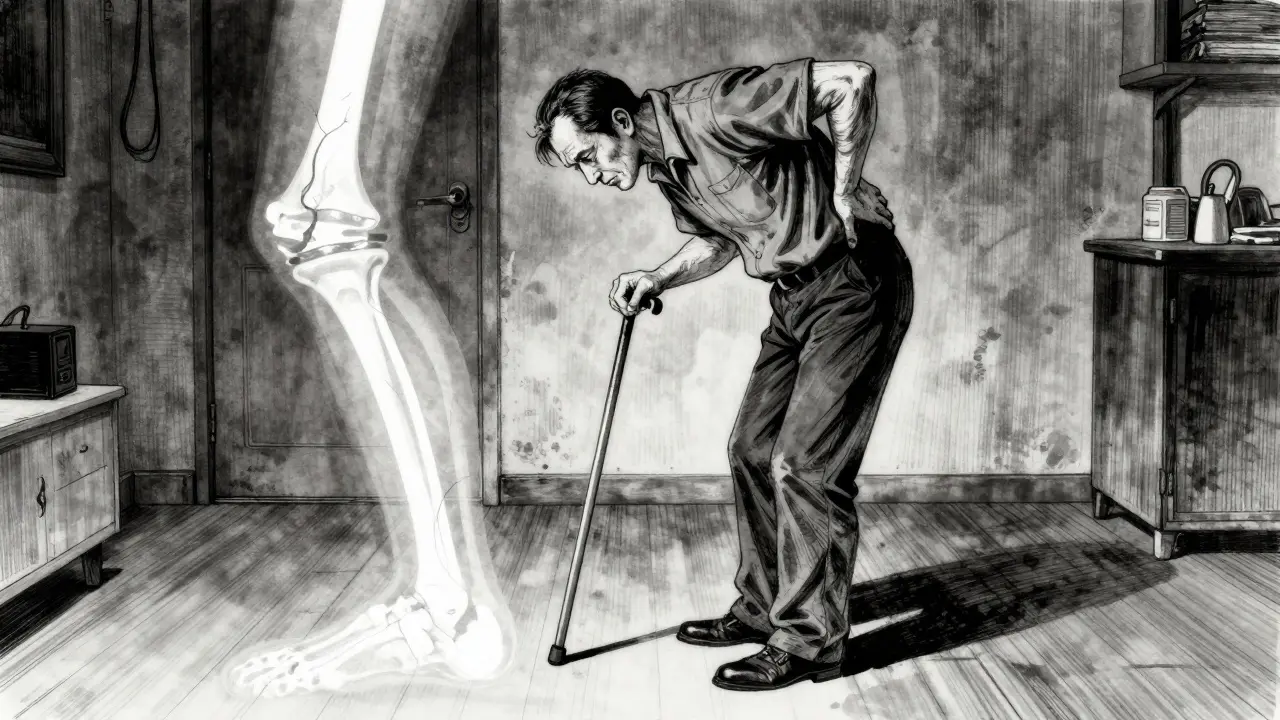
When your lower back aches after standing too long, or your hamstrings feel tight no matter how much you stretch, it might not just be a bad posture or a pulled muscle. For about 6 in every 100 adults, especially those over 50, that pain could be spondylolisthesis-a condition where one of the vertebrae in your spine slips forward over the one below it. It’s not rare. It’s not always dramatic. But when it causes pain or instability, it changes how you move, sit, and live.
What Exactly Is Spondylolisthesis?
Spondylolisthesis comes from Greek: spondylo means vertebra, and olisthesis means to slip. So, it’s exactly what it sounds like-one bone in your spine slides out of place. Most often, this happens between the fifth lumbar vertebra (L5) and the first sacral bone (S1). That’s the spot where your lower spine meets your pelvis, and it takes a lot of stress every day when you stand, walk, or lift. The slippage is measured as a percentage using the Meyerding scale. Grade I is less than 25% slippage, Grade II is 25-50%, Grade III is 50-75%, and Grade IV is over 75%. Most cases (about 75%) are Grade I or II. But even a small slip can cause big problems if it presses on nerves or destabilizes your spine. There are five main types, each with a different cause:- Degenerative: The most common in adults over 50. Arthritis wears down the discs and joints, letting the vertebra slip. This accounts for about 65% of adult cases.
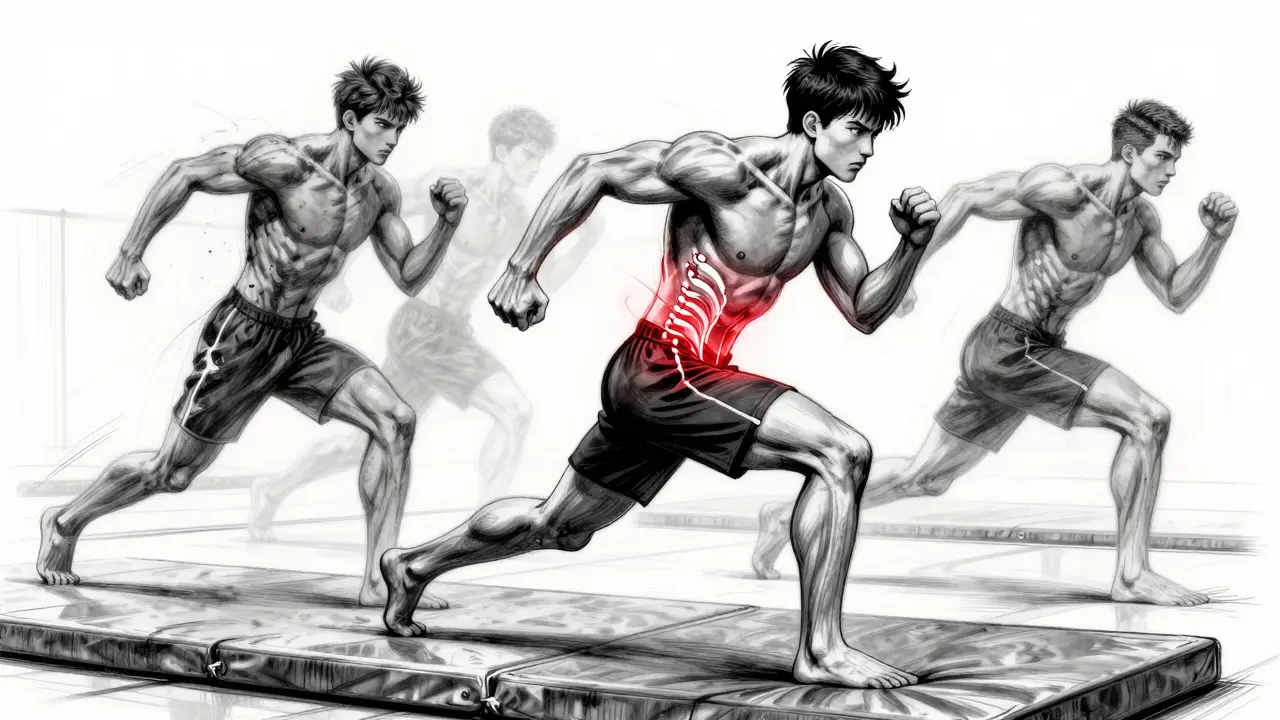
- Isthmic: Caused by a stress fracture in a small bone segment called the pars interarticularis. Common in teens and young athletes who do a lot of back-bending-think gymnasts, football linemen, or weightlifters.
- Dysplastic: A birth defect where the spinal joints don’t form properly. Often shows up in kids under 6.
- Pathologic: Caused by diseases like osteoporosis, tumors, or infections that weaken the bone.
- Traumatic: From a sudden injury, like a fall or car crash, that breaks part of the vertebra.
Why Does It Hurt? The Real Symptoms
Here’s the thing: almost half of people with spondylolisthesis feel nothing at all. Their slip shows up on an X-ray, but they never have pain. That’s why it’s often found by accident. But when symptoms do appear, they’re usually predictable:- Lower back pain that feels like a deep ache or muscle strain. It gets worse when you stand or walk and improves when you sit or bend forward.
- Buttock and thigh pain-not always sharp sciatica, but a dull, heavy pressure that runs down the back of the leg.
- Tight hamstrings. About 70% of people with symptoms can’t touch their toes. Stretching helps, but it doesn’t fix the root problem.
- Stiffness and trouble walking. You might feel like your spine is “giving out” after a few blocks.
- Numbness or weakness in one or both legs. This happens in about 35% of high-grade slips (Grade III or IV), when the slipped bone pinches a nerve root.
How Is It Diagnosed?
You won’t know just by feeling it. You need imaging:- Standing lateral X-rays are the first step. They show how far the vertebra has slipped and whether it’s stable or moving with motion.
- CT scans give a detailed look at the bone-perfect for spotting fractures in the pars interarticularis, especially in younger patients.
- MRI shows the soft stuff: discs, ligaments, and nerves. It tells you if a nerve is compressed and how much inflammation or disc degeneration is happening.
Conservative Treatment: What Works Before Surgery
Most people don’t need surgery. In fact, about 80% of cases improve with non-surgical care. The goal? Reduce pain, stabilize the spine, and restore movement. Here’s how:- Activity modification: Avoid heavy lifting, back-bending, or high-impact sports. If you’re a runner or cyclist, switching to swimming or elliptical training can help.
- Physical therapy: A 12- to 16-week program focused on core strengthening (transverse abdominis, multifidus) and hamstring stretching is the gold standard. Studies show 65% of people stick with it long enough to see results.
- NSAIDs: Ibuprofen or naproxen can help with inflammation and pain, but they don’t fix the slip. Use them short-term.
- Epidural steroid injections: If nerve pain is sharp and shooting, a steroid shot near the affected nerve can calm things down for weeks or months. It’s not a cure, but it can buy time for therapy to work.
Fusion Surgery: The Options When Things Don’t Improve
Surgery is considered when conservative care fails after 6-12 months and pain is disabling. The main goal? Stop the slip from getting worse and relieve pressure on nerves. The most common procedure is spinal fusion-joining two vertebrae together so they heal into one solid bone. There are three main fusion techniques:- Posterolateral fusion (PLF): Bone graft is placed along the back of the spine, outside the spinal canal. It’s the oldest method, used in about 55% of cases. Success rate for Grade I-II slips: 75-85%. For higher grades, it drops to 60-70%.
- Interbody fusion (PLIF/TLIF): The disc between the two vertebrae is removed and replaced with a spacer filled with bone graft. This restores disc height and opens up the space where nerves exit the spine. Used in about 35% of cases. Success rate: 85-92% across all grades. This is now the preferred method for most surgeons.
- Minimally invasive fusion (MIS): Smaller incisions, less muscle damage. Used in about 10% of cases. Recovery is faster, but not everyone is a candidate. It’s best for Grade I-II slips without major instability.

What Happens After Surgery?
Fusion isn’t a quick fix. Recovery takes time:- First 6-8 weeks: No lifting, twisting, or bending. You’ll need help with daily tasks.
- Months 3-6: Physical therapy focuses on walking, posture, and gentle core work.
- Full recovery: 12-18 months. That’s when the bone fully fuses and you can return to most activities.
Newer Options and What’s Coming
Fusion isn’t the only path anymore. In 2022, the FDA approved two new interbody devices designed specifically for spondylolisthesis. Early results show 89% fusion rates at 6 months-better than older models. Some surgeons are now using bone morphogenetic protein (BMP) or stem cell grafts to boost fusion success. A 2023 trial found BMP-2 raised fusion rates to 94% in high-risk patients, compared to 81% with traditional bone grafts. For younger, active patients with mild slips, dynamic stabilization devices are being tested. These let the spine move a little, unlike fusion. But long-term data is still limited. After 5 years, they’re about 76% successful-still below fusion’s 88%. There’s also new research on predicting who will benefit from surgery. A 2023 study identified 11 clinical and imaging factors-like disc height loss, facet joint degeneration, and hamstring tightness-that can predict surgical outcomes with 83% accuracy. That means fewer people get unnecessary operations.What You Can Do Right Now
If you’re dealing with lower back pain that won’t go away:- Don’t ignore it. See a doctor if it lasts more than 3-4 weeks.
- Get an X-ray. Don’t skip the standing lateral view-it’s the most telling.
- Start physical therapy. Even if you’re not sure about surgery, core and hamstring work helps.
- Quit smoking. Smokers are 3.2 times more likely to have fusion failure.
- Manage your weight. A BMI over 30 increases surgical complications by 47%.