SGLT2 Inhibitor Side Effects: Dehydration, Dizziness, and Blood Pressure Changes Explained
 Nov, 16 2025
Nov, 16 2025
SGLT2 Inhibitor Hydration & Blood Pressure Calculator
Calculate Your Fluid Balance
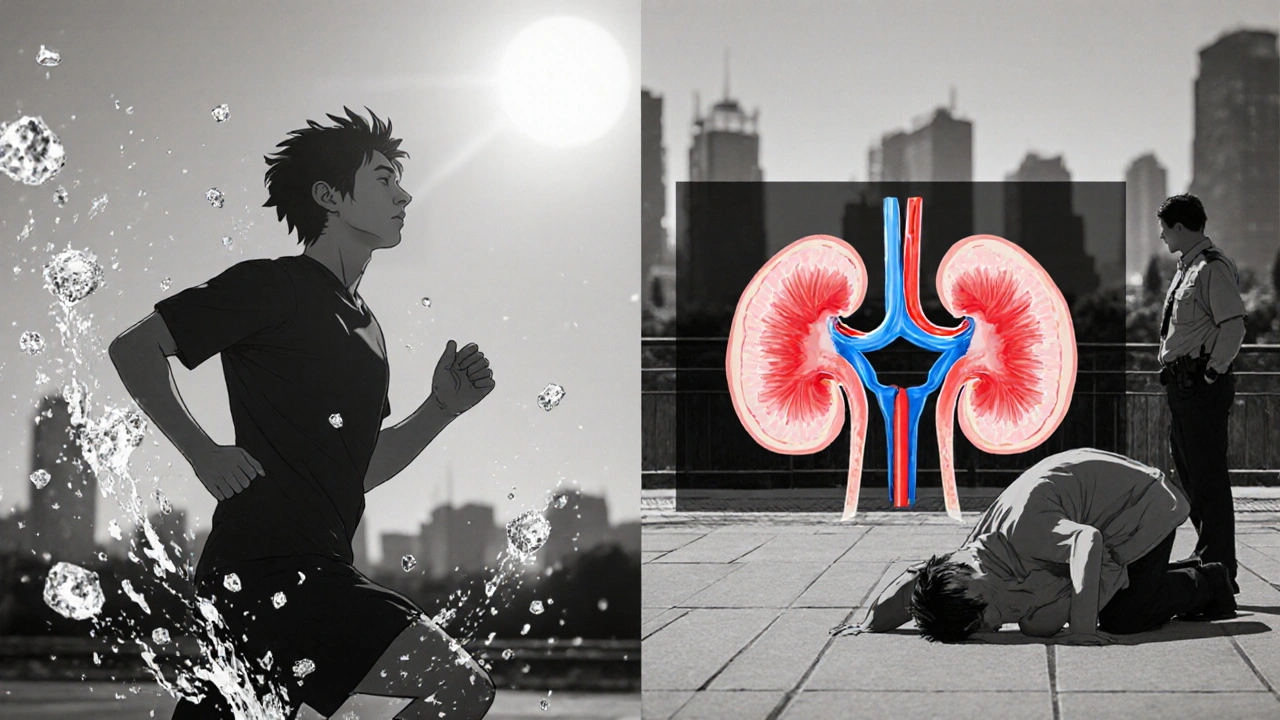
When you start taking an SGLT2 inhibitor like empagliflozin, Farxiga, or Invokana, you’re not just lowering your blood sugar-you’re also changing how your body handles fluid and pressure. These drugs, originally designed for type 2 diabetes, have become go-to treatments for heart failure and kidney disease too. But with those benefits come real side effects: dehydration, dizziness, and drops in blood pressure. If you’re new to these meds or thinking about starting them, you need to know what’s really happening inside your body-and how to stay safe.
How SGLT2 Inhibitors Work Like Natural Diuretics
SGLT2 inhibitors don’t work like insulin or metformin. Instead, they trick your kidneys into spilling glucose into your urine. Normally, your kidneys reabsorb almost all the sugar filtered from your blood. But these drugs block that process, forcing 70-100 grams of glucose out each day. That’s about 250-400 extra calories lost daily-no dieting needed.
Here’s the catch: glucose doesn’t leave alone. It pulls sodium and water with it. That’s why SGLT2 inhibitors act like mild diuretics. You’re not just peeing out sugar-you’re losing 1-1.5 liters of fluid in the first week. That’s the same as skipping a couple of meals and drinking less water. It’s why many people lose 1.5-2.5 kg (3-5 lbs) quickly after starting.
This isn’t a bug-it’s the feature. Less fluid means lower pressure in your blood vessels. That’s why these drugs lower systolic blood pressure by 4-6 mmHg on average. For someone with high blood pressure or heart failure, that’s a win. But for others, especially older adults or those already on blood pressure meds, it can be risky.
Why Dehydration Happens-And Who’s at Risk
Dehydration from SGLT2 inhibitors isn’t rare. Clinical trials show 1.3% to 2.8% of users experience volume depletion symptoms like dry mouth, dark urine, fatigue, or fainting. That’s 2-3 times higher than placebo. In real life, it’s often worse.
Here’s who’s most vulnerable:
- People over 65-thirst signals weaken with age, so you might not notice you’re drying out
- Those on diuretics (like furosemide) or ACE inhibitors-double the fluid loss
- People with eGFR below 60-kidneys can’t compensate as well
- Anyone in hot weather, exercising, or sick with vomiting/diarrhea
A 72-year-old man on Jardiance and lisinopril started feeling lightheaded after a walk in 28°C weather. His blood pressure dropped to 92/58. He didn’t drink extra water because he didn’t feel thirsty. Within days, he was hospitalized for dehydration. This isn’t an outlier-it’s a common story in primary care clinics.
Unlike regular diuretics, SGLT2 inhibitors don’t cause potassium loss. But they do make your body less able to hold onto sodium and water. If you’re not drinking enough, your volume drops fast. And once you’re dehydrated, your kidneys can’t recover without help.
Dizziness: It’s Not Just ‘Feeling Off’-It’s Orthostatic Hypotension
Dizziness is the most reported side effect after dehydration. Around 4-6% of people on SGLT2 inhibitors feel lightheaded, especially when standing up. That’s not normal aging-it’s orthostatic hypotension: your blood pressure plummets when you move from sitting to standing.
Studies show 63% of dizziness cases are tied to this. Your systolic pressure can drop 20 mmHg or more. That’s enough to make you see stars, feel wobbly, or even fall. In one study, patients with baseline systolic pressure under 130 mmHg were nearly three times more likely to get dizzy.
Canagliflozin has the highest dizziness rate-6.3 cases per 1,000 patient-years. Empagliflozin and dapagliflozin are slightly lower. But the timing is the same: 78% of cases happen in the first four weeks. That’s when fluid loss peaks.
Real-world reports on Reddit and Drugs.com confirm this. One user wrote: “Started Jardiance last week. Got dizzy standing up. Thought it was stress. Turned out my BP was 88/54.” Another: “I thought I was just getting old-until my doctor said it was the med.”
The good news? Most cases are mild and fade after 2-4 weeks as your body adjusts. But if you’re dizzy every time you stand, or if it’s affecting your balance, you need to act.

How Blood Pressure Drops-And Why It’s a Double-Edged Sword
SGLT2 inhibitors lower blood pressure in two ways. First, they reduce preload: less fluid in your veins means less pressure pushing back on your heart. Second, they reduce afterload: blood vessels relax because of improved endothelial function and less arterial stiffness.
That’s why these drugs work so well in heart failure. Less pressure on the heart means less strain. In the EMPEROR-Reduced trial, empagliflozin cut heart failure hospitalizations by 30%-even in people without diabetes.
But here’s the flip side: if your blood pressure was already low (below 120 mmHg systolic), this drop can be dangerous. One study found patients with baseline SBP under 120 had a 3.2-fold higher risk of symptomatic hypotension. That’s why doctors now check your blood pressure before prescribing these drugs.
It’s not just about the number. It’s about how you feel. If you’re dizzy, tired, or have blurred vision when standing, your BP might be too low-even if the monitor says 110/70. That’s why orthostatic checks (measuring BP lying and standing) are now standard at the 1-week follow-up.
And here’s something surprising: the blood pressure drop happens whether you have diabetes or not. That’s why these drugs are now approved for heart failure in non-diabetic patients too. The benefit isn’t tied to sugar-it’s tied to fluid and vessel health.
How to Stay Safe: Practical Tips for Patients and Doctors
If you’re on or starting an SGLT2 inhibitor, here’s what you need to do:
- Drink more water. Add 500-1,000 mL (2-4 cups) extra daily, especially in heat or after exercise. Don’t wait until you’re thirsty.
- Check your blood pressure. Take it lying down and then standing. If your systolic drops more than 20 mmHg or you feel dizzy, call your doctor.
- Monitor your weight. A sudden drop of more than 2 kg in a week means you’re losing too much fluid.
- Hold the dose if you’re sick. If you have vomiting, diarrhea, or fever, pause the med until you’re eating and drinking normally.
- Don’t rush the dose. Start with the lowest dose (e.g., empagliflozin 10 mg instead of 25 mg) if you’re older, on other BP meds, or have kidney issues.
- Don’t stop cold turkey. The cardiovascular benefits are strong. If dizziness is mild, your doctor may lower your diuretic dose instead of stopping the SGLT2 drug.
Doctors should screen for these risks before prescribing. Check kidney function, baseline BP, and current meds. Schedule a follow-up at 7-10 days. Most side effects are manageable-if caught early.
When to Worry: Red Flags That Need Immediate Attention
Not all dizziness or dry mouth is harmless. Call your doctor or go to urgent care if you have:
- Confusion or difficulty thinking clearly
- Very dark urine or not peeing for 12+ hours
- Heart palpitations or chest pain
- Systolic BP below 90 mmHg
- Fainting or near-fainting episodes
These aren’t normal side effects-they’re signs of severe volume depletion. Left untreated, they can lead to acute kidney injury or shock. It’s rare, but it happens.
One 78-year-old woman on dapagliflozin and hydrochlorothiazide stopped drinking water because she was “afraid of peeing too much.” She developed kidney failure and had to be hospitalized. She didn’t realize the meds were working too well.
Bottom Line: Benefits Outweigh Risks-If You’re Careful
SGLT2 inhibitors are among the most important diabetes drugs developed in the last decade. They don’t just lower sugar-they protect your heart, kidneys, and blood vessels. In trials, they’ve saved lives. For people with heart failure, one in six avoids death or hospitalization because of them.
But they’re not magic. They’re powerful tools that require smart use. Dehydration, dizziness, and low blood pressure aren’t side effects you ignore. They’re signals. Listen to them. Adjust. Talk to your doctor. Drink water. Check your BP.
If you’re taking one of these meds, you’re not just managing diabetes-you’re managing your body’s fluid balance. That’s a responsibility. But with the right knowledge, it’s a manageable one.
Robert Merril
November 18, 2025 AT 06:47So these drugs make you pee out sugar like a diabetic sprinkler system and wonder why you feel like a dried prune? Classic pharma magic. I started on Jardiance and lost 4 lbs in 3 days. Thought I hit the lottery. Turns out I was just dehydrated and about to pass out in the shower. Doc said drink more water. Yeah thanks captain obvious
Noel Molina Mattinez
November 20, 2025 AT 06:09My grandma took this and stopped drinking because she was scared of peeing too much then ended up in the hospital. They didn’t even tell her to drink more. Just said it’s normal. Normal is not when you can’t stand up without seeing stars
Roberta Colombin
November 20, 2025 AT 08:00I want to thank the author for writing this with such care. Many people are scared to ask questions about their medications, and this guide gives clear, kind advice. If you’re new to SGLT2 inhibitors, please take a breath and read this slowly. Your body is trying to tell you something. Drink water. Check your blood pressure. Talk to your doctor. You are not alone in this journey.
Dave Feland
November 20, 2025 AT 11:25Let’s be clear: this is not medicine. This is corporate pharmacology disguised as innovation. SGLT2 inhibitors were never designed for heart failure. They were a failed diabetes drug repackaged with a PR campaign funded by Big Pharma. The real side effect? Profit margins. The FDA approved this because they’re underfunded and overworked. And now millions of elderly patients are being turned into human diuretics. Wake up.
Ashley Unknown
November 21, 2025 AT 04:09Okay so I just want to say this is the most terrifying thing I’ve ever read. I’ve been on Farxiga for 6 months and I thought the dizziness was just stress or aging. Turns out I was one hot shower away from collapsing in the bathroom. My husband found me on the floor. I didn’t even cry. I just stared at the tiles. That’s when I knew something was wrong. And now I’m terrified to take any more pills. What if this is just the beginning? What if next they make me lose my kidneys? What if they start adding more diuretics to my cocktail? I’m 58 and I just want to sit on my porch and drink tea without feeling like my blood is being siphoned out of me. I’m not even diabetic. I was prescribed this for ‘pre-diabetes’ and now I’m a walking dehydration experiment
Georgia Green
November 21, 2025 AT 14:12I started empagliflozin last month. Lost 3 lbs. Got dizzy standing up. Didn’t think much of it. Then I checked my BP and it was 94/56. Called my doc. They lowered my lisinopril. Now I drink 2 extra glasses of water a day and I’m fine. Don’t panic. Just pay attention. Your body knows.
Christina Abellar
November 22, 2025 AT 18:00Drink water. Check BP. Listen to your body. Simple. Done.
Eva Vega
November 24, 2025 AT 11:30The hemodynamic modulation induced by SGLT2 inhibition results in a significant reduction in intravascular volume, leading to a compensatory decrease in preload and afterload. This is mechanistically distinct from loop diuretics, as it preserves electrolyte homeostasis while promoting natriuresis. Clinical monitoring of orthostatic vitals is therefore essential during titration phases.
Matt Wells
November 24, 2025 AT 20:51While the article presents a reasonable clinical overview, it fails to acknowledge the significant confounding variables present in real-world prescribing. The data cited is largely drawn from industry-sponsored trials with strict exclusion criteria. In primary care, where polypharmacy and frailty are the norm, these side effects are grossly underreported. The authors’ tone is dangerously reassuring.
Margo Utomo
November 25, 2025 AT 02:48Y’all need to hydrate like your life depends on it… because it kinda does 💧😂 I started on Invokana and thought I was dying. Turned out I just needed to chug water like it was my job. Now I carry a bottle everywhere. My BP is stable, my kidneys are happy, and I’m not passing out in the grocery store. You got this! 🙌
George Gaitara
November 25, 2025 AT 03:52This article is just a glorified ad. If these drugs were so safe, why are people ending up in the ER? Why are doctors quietly prescribing lower doses? Why are pharmacies putting warning stickers on the bottles? They know. They just don’t want to admit it. This is a slow poisoning disguised as progress. Wake up.
Deepali Singh
November 25, 2025 AT 09:03Statistical analysis of the EMPA-REG OUTCOME trial reveals a 1.8% absolute increase in volume depletion events among SGLT2 inhibitor users compared to placebo. However, the relative risk is confounded by concomitant diuretic use, which increases the hazard ratio to 2.9. The article omits this interaction. Also, the weight loss cited is likely due to glycogen depletion, not purely fluid loss. Misleading.
Sylvia Clarke
November 25, 2025 AT 13:37It’s fascinating how we’ve turned a metabolic intervention into a lifestyle gamble. These drugs don’t just lower glucose-they rewire your body’s relationship with water, pressure, and survival instinct. And yet, we hand them out like candy. We tell people to drink more water, but we don’t teach them how to listen to thirst. We measure BP, but we don’t teach orthostatic awareness. We treat symptoms, not systems. The real failure isn’t the drug-it’s the system that lets you start it without a single conversation about hydration.
Jennifer Howard
November 26, 2025 AT 10:34I am absolutely appalled by the negligence here. People are dying because they are not being properly educated. This is not a minor side effect. This is medical malpractice. You should be required to attend a 2-hour seminar before being prescribed this. And doctors who prescribe it without checking kidney function and baseline BP should lose their licenses. I’ve seen patients collapse. I’ve seen families cry. This is not science. This is negligence dressed in white coats.
Abdul Mubeen
November 28, 2025 AT 09:28While the article is well-structured, it lacks critical engagement with the broader geopolitical implications of pharmaceutical patent monopolies. The global South bears disproportionate risk from these agents due to limited access to monitoring infrastructure. The fact that these drugs are marketed aggressively in low-resource settings while the side effect profiles remain under-discussed is ethically indefensible.