Pulmonary Embolism: Sudden Shortness of Breath and How It’s Diagnosed
 Jan, 7 2026
Jan, 7 2026
One minute you’re walking up the stairs, and the next, you can’t catch your breath. No asthma attack. No panic attack. Just pure, unexplained gasping for air. If this happened to you - especially if it came out of nowhere - you might be dealing with something far more dangerous than you think: a pulmonary embolism.
What Exactly Is a Pulmonary Embolism?
A pulmonary embolism (PE) happens when a blood clot breaks loose, travels through your veins, and gets stuck in one of the arteries in your lungs. It’s not just a blockage - it’s a sudden cutoff of blood flow to part of your lung. Without that blood flow, your body can’t get enough oxygen. That’s why breathing becomes so hard, so fast. Most of these clots start in the deep veins of your legs - a condition called deep vein thrombosis (DVT). About 70% of all PEs come from clots that formed in the lower limbs. Less often, they come from veins in the arms, especially after a catheter was placed. Once that clot moves, it doesn’t care how healthy you are. Even young, active people can get hit. Every year in the U.S., around 60 to 70 people out of every 100,000 develop a pulmonary embolism. And about 100,000 die from it. Many of those deaths happen because no one recognized the signs early enough.Why Sudden Shortness of Breath Is the Biggest Red Flag
If you remember just one thing about PE, remember this: sudden shortness of breath is the #1 warning sign. In fact, 85% of people with PE report this symptom. It’s not gradual. It’s not "I’m just tired." It’s "I can’t breathe, even when I’m sitting still." The severity depends on how big the clot is. A large clot blocking a main artery causes extreme, terrifying breathlessness - even at rest. Smaller clots might just make you feel winded climbing one flight of stairs. But either way, it’s not normal. Other symptoms often show up too:- Chest pain that gets worse when you breathe in or cough (74% of cases)
- A dry cough, sometimes with blood (23% have coughing up blood)
- One leg swollen, warm, or tender (44% have DVT signs)
- Rapid heartbeat (over 100 bpm in 30% of cases)
- Fainting or dizziness (14% of cases)
- Fast breathing (more than 20 breaths per minute in over half)
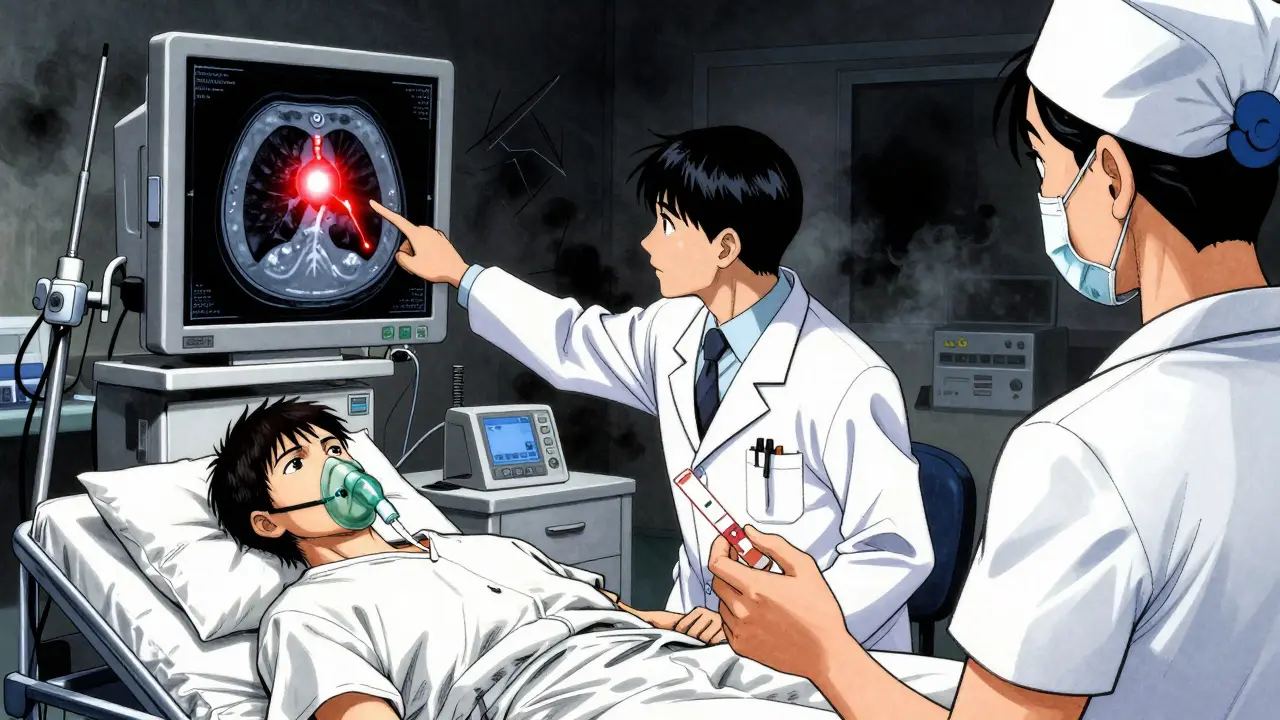
How Doctors Diagnose It - Step by Step
There’s no single test that confirms PE right away. Diagnosis is a puzzle. Doctors piece it together using your symptoms, risk factors, and a few key tests. Step 1: Clinical Probability ScoringBefore any blood work or scans, doctors use tools like the Wells Score or Geneva Score. These aren’t guesswork - they’re evidence-based checklists. Points are added for things like:
- Recent surgery or immobilization
- History of DVT or PE
- Heart rate over 100
- Leg swelling
- Alternative diagnosis being unlikely
D-dimer is a protein fragment released when a clot breaks down. If the level is normal and you’re low-risk, PE is almost certainly ruled out - 97% accurate in that group. But here’s the catch: if you’re over 50, pregnant, have cancer, or just had surgery, D-dimer can be high even without a clot. That’s why it’s not a standalone test for older adults. In fact, its accuracy drops from 94% to just 54% specificity in people over 50. So if the D-dimer is high, you still need imaging. Step 3: CT Pulmonary Angiography (CTPA)
This is the gold standard. You get an IV with contrast dye, then a fast CT scan of your chest. It shows exactly where the clot is. It finds PE in 95% of cases and misses only 4%. The scan takes less than 10 minutes. Radiation exposure is low - about the same as a year of natural background radiation. But it’s not for everyone. People with kidney problems or severe allergies to iodine may not be candidates. Step 4: Ultrasound for DVT
If the CTPA isn’t possible, doctors often check your legs with a compression ultrasound. If they find a clot in your thigh or calf, and you have symptoms like shortness of breath, they’ll treat you for PE even without a lung scan. Why? Because the chance of a clot traveling is so high - over 90% accurate for detecting dangerous clots. Step 5: V/Q Scan (When CTPA Isn’t an Option)
This test compares air flow and blood flow in your lungs. It’s used when someone can’t have contrast dye or has kidney failure. It’s 85% sensitive - good, but not as precise as CTPA. It’s also harder to find because only 78% of major hospitals have the nuclear medicine equipment needed.
When Time Is Critical: Emergency Signs
Some people don’t just get short of breath - they go into shock. That’s massive PE. Signs include:- Low blood pressure
- Blue lips or fingers
- Confusion or passing out
- Extreme rapid heartbeat
Who’s at Highest Risk?
You might think PE only happens to older people or those in hospitals. But risk factors are everywhere:- Cancer patients: 4.7 times more likely to get PE. Chemotherapy and tumors make blood clot easier.
- Recent surgery or trauma: Especially hip, knee, or abdominal operations.
- Long flights or bed rest: Sitting still for 4+ hours increases risk.
- Birth control or hormone therapy: Estrogen raises clotting risk.
- Family history of clots: Genetic conditions like Factor V Leiden.
- Previous PE or DVT: One in three people with a past clot will get another within 10 years.
What’s Changing in Diagnosis Today?
The field is evolving. New tools are making diagnosis faster and smarter.- Age-adjusted D-dimer: Now, the "normal" level goes up with age. For someone 70, the cutoff is 700 ng/mL instead of 500. This cuts down unnecessary scans by over a third.
- AI in CT scans: Algorithms like PE-Flow can spot tiny clots in CTPA scans with 96% accuracy - faster than human radiologists.
- Pulmonary Embolism Response Teams (PERT): These are specialized teams of doctors (pulmonologists, cardiologists, hematologists) who respond together to severe cases. Hospitals with PERT have seen mortality drop by over 4%.
- New blood markers: Researchers are testing combinations of proteins like thrombomodulin and plasmin-antiplasmin. Early results show 98.7% accuracy in ruling out PE in intermediate-risk patients.
What Happens After Diagnosis?
If you’re diagnosed with PE, you’ll start anticoagulants - blood thinners - right away. Common ones include rivaroxaban, apixaban, or warfarin. Most people take them for at least 3 months. Some need them longer - especially if they have cancer or a genetic clotting disorder. You’ll also get advice on movement. No more sitting for hours. No more long flights without compression socks. Walking every hour, staying hydrated, and avoiding prolonged immobility are key. Follow-up scans aren’t always needed unless symptoms return. But if you’ve had one PE, you’re at higher risk for another. That’s why doctors stress lifelong awareness.What to Do If You Suspect PE
If you or someone you know has sudden shortness of breath - especially with chest pain, leg swelling, or dizziness - don’t wait. Don’t assume it’s anxiety or asthma. Go to the ER. Say clearly: "I think I might have a pulmonary embolism." Bring a list of recent surgeries, travel, medications, or family history of clots. That info saves time. Hospitals with structured PE pathways have cut diagnosis time from over two hours to under 45 minutes. That’s the difference between life and death.Final Thought: Don’t Ignore the Breath
Breathlessness is one of the body’s loudest alarms. When it comes out of nowhere, it’s not just fatigue. It’s not just stress. It could be a clot silently blocking your lung. The good news? If caught early, PE is treatable. Most people recover fully. The danger isn’t the clot itself - it’s the delay. Know the signs. Speak up. Push for answers. Your lungs are counting on it.Can you have a pulmonary embolism without knowing it?
Yes, but it’s rare. Small clots in the outer edges of the lungs might cause mild symptoms like slight breathlessness or a dry cough that fades quickly. These can be mistaken for a cold or allergies. However, even small clots carry risk - they can grow or break off again. Most people with PE notice at least some warning signs, even if they don’t recognize them as serious.
Is a pulmonary embolism the same as a heart attack?
No. A heart attack happens when a clot blocks blood flow to the heart muscle. A pulmonary embolism blocks blood flow to the lungs. The chest pain can feel similar - sharp and worse with breathing - but the organs affected are different. Heart attacks often cause nausea, sweating, and arm pain. PE usually causes sudden shortness of breath and sometimes leg swelling. The treatments are also different.
Can you get a pulmonary embolism from sitting too long on a flight?
Yes. Sitting still for more than 4 hours - whether on a plane, car, or train - slows blood flow in the legs, increasing clot risk. This is called "economy class syndrome," though it can happen in any seat. Moving your legs, wearing compression socks, and staying hydrated reduce the risk. For high-risk people, doctors may recommend a blood thinner before long travel.
Does a negative D-dimer test mean I definitely don’t have a pulmonary embolism?
Only if you’re low-risk. If you have no risk factors and your D-dimer is normal, PE is extremely unlikely - less than 1% chance. But if you’re over 50, have cancer, just had surgery, or have other risk factors, a negative D-dimer doesn’t rule it out. Doctors will still order a CT scan if symptoms are strong.
How long do you need to take blood thinners after a pulmonary embolism?
It depends. Most people take them for at least 3 months. If the clot was caused by a temporary trigger - like surgery or a long flight - you may stop after that. But if you have cancer, a genetic clotting disorder, or had more than one PE, you might need to take them for life. Your doctor will decide based on your individual risk of recurrence.
Can exercise help prevent another pulmonary embolism?
Yes - but not immediately after diagnosis. After starting blood thinners, light walking is encouraged to improve circulation. Once stable, regular aerobic exercise like brisk walking, swimming, or cycling helps prevent future clots by keeping blood moving. Avoid heavy lifting or contact sports until cleared by your doctor, especially if you’re on anticoagulants.
Joanna Brancewicz
January 8, 2026 AT 00:25Sudden dyspnea + unilateral leg edema = PE until proven otherwise. D-dimer’s useless in post-op or cancer patients-don’t waste time. CTPA’s gold standard. If contraindicated, go straight to leg US. No guesswork.
Time is lung tissue.
Lois Li
January 8, 2026 AT 16:28I’ve seen this happen to my sister after her knee surgery. They told her it was anxiety for three weeks. She almost didn’t make it to the ER. Please, if you feel like you’re drowning while sitting still, say the words out loud: I think it’s a clot. It’s not dramatic. It’s medical.
Doctors need to hear it. We need to say it.
Prakash Sharma
January 8, 2026 AT 20:35Why are we letting Americans treat PE like a myth? In India, we know clotting kills fast. No waiting for second opinions. No ‘maybe it’s stress.’ You get scanned or you die. This post is good, but the system here is broken. We need mandatory PE protocols in every ER. Not optional.
Donny Airlangga
January 9, 2026 AT 04:58My mom had a PE after her hip replacement. They missed it for 48 hours because her D-dimer was ‘only slightly elevated.’ She was in the ICU for a week. I wish I’d known then what I know now. This post saved my life. Thank you.
Now I tell everyone: if you’re short of breath and it came out of nowhere-go. Now.
Evan Smith
January 9, 2026 AT 23:09So let me get this straight… you’re telling me I can’t sit on a flight for 8 hours without becoming a walking blood clot? And the solution is… walking? Wow. Who knew? Next you’ll tell me smoking causes cancer.
Also, why is this a 10,000-word essay and not a poster in every airport bathroom?
Manish Kumar
January 11, 2026 AT 08:02Think about it: the body is a river, and clots are stones. When the flow stops, the stones settle. But we don’t ask why the river stopped. We just try to remove the stone. We treat the symptom, not the silence between breaths. The real question isn’t how to diagnose PE-it’s why we’ve forgotten how to listen to our own bodies. We’ve outsourced sensation to algorithms and D-dimer values. But the body still screams. We just don’t hear it anymore.
Maybe the clot isn’t in the lung. Maybe it’s in our collective denial.
Kristina Felixita
January 12, 2026 AT 19:01OMG I JUST REALIZED-my cousin had this and we thought she was just ‘overworked’!! She was on a 12-hour flight, then passed out at the airport… they thought it was a panic attack!!
She’s fine now, thank god, but she’s on blood thinners forever. I’m sending this to EVERYONE I know. PLEASE, if you’re flying, move your ankles, drink water, and don’t ignore that weird ‘can’t catch breath’ feeling. It’s not ‘just tired.’
Share this. Save a life. #PEawareness
Ken Porter
January 14, 2026 AT 03:10Another liberal health post. Real men don’t get PE. They get back up. This is why America’s healthcare is broken-overtesting, overdiagnosing, overmedicating. If you’re short of breath, tough it out. Walk it off. Stop coddling people with CT scans and anticoagulants.
Also, D-dimer? Please. My grandpa didn’t have a CT scan in 1972 and he lived to 92.
swati Thounaojam
January 14, 2026 AT 08:39My aunt had PE after her C-section. No one knew. She just kept saying she was tired. Now she’s okay but scared to fly. I’m telling everyone: if you had a baby, move your legs. Seriously.
Dave Old-Wolf
January 15, 2026 AT 09:34I had a PE after a 14-hour drive home from college. I thought I was just out of shape. Took me two weeks to finally go to the ER. They said I was lucky I didn’t collapse on the highway.
Now I walk every hour on road trips. I wear socks. I drink water. I tell my friends. It’s not a big deal. It’s just common sense.
Why is this even a debate?
Molly Silvernale
January 16, 2026 AT 00:48There’s poetry in the way breath fails-sudden, silent, like a candle snuffed by a gust you didn’t feel coming. We call it a clot. But it’s not a clot. It’s the universe whispering: you forgot to move. You forgot to breathe-not just air, but rhythm, motion, life.
And yet-we still sit. Still fly. Still ignore. Until the silence becomes a scream.
Maybe the real diagnosis isn’t in the CT scan. Maybe it’s in the shame of having waited too long to ask for help.
christy lianto
January 16, 2026 AT 06:07My nurse friend says PE is the silent killer that walks into ERs every day. She’s seen it-people laughing at the front desk, then collapsing 20 minutes later. No warning. No drama. Just… gone.
Don’t be the person who says ‘I thought it was anxiety.’ Be the person who says ‘I’m not breathing right.’
And yes, I’m telling my mom to wear socks on her flight to Florida.
Annette Robinson
January 16, 2026 AT 09:31As a healthcare educator, I want to thank you for this comprehensive, accurate, and compassionate overview. This is exactly the kind of patient-facing content that saves lives. I’ve shared it with my entire nursing program. The inclusion of age-adjusted D-dimer and PERT teams shows true clinical depth.
Keep doing this work.
Luke Crump
January 17, 2026 AT 17:00Let’s be real: this entire post is just fear-mongering dressed up as medicine. What’s next? Are we gonna panic about every cough? PE is rare. You’re more likely to die from a vending machine falling on you.
And CTPA? Radiation? Contrast? You’re trading one risk for ten. I’d rather die quietly than get scanned into oblivion.
Also, who gave you a medical license, anyway?
Aubrey Mallory
January 18, 2026 AT 08:26My sister-in-law had a PE after her third child. She didn’t even know she was at risk. I’m starting a local support group for postpartum women. If you’ve had a baby in the last 6 weeks and you’re short of breath-don’t wait. Don’t apologize. Say it. Go. We’re in this together.
And if you’re reading this-you’re not alone.