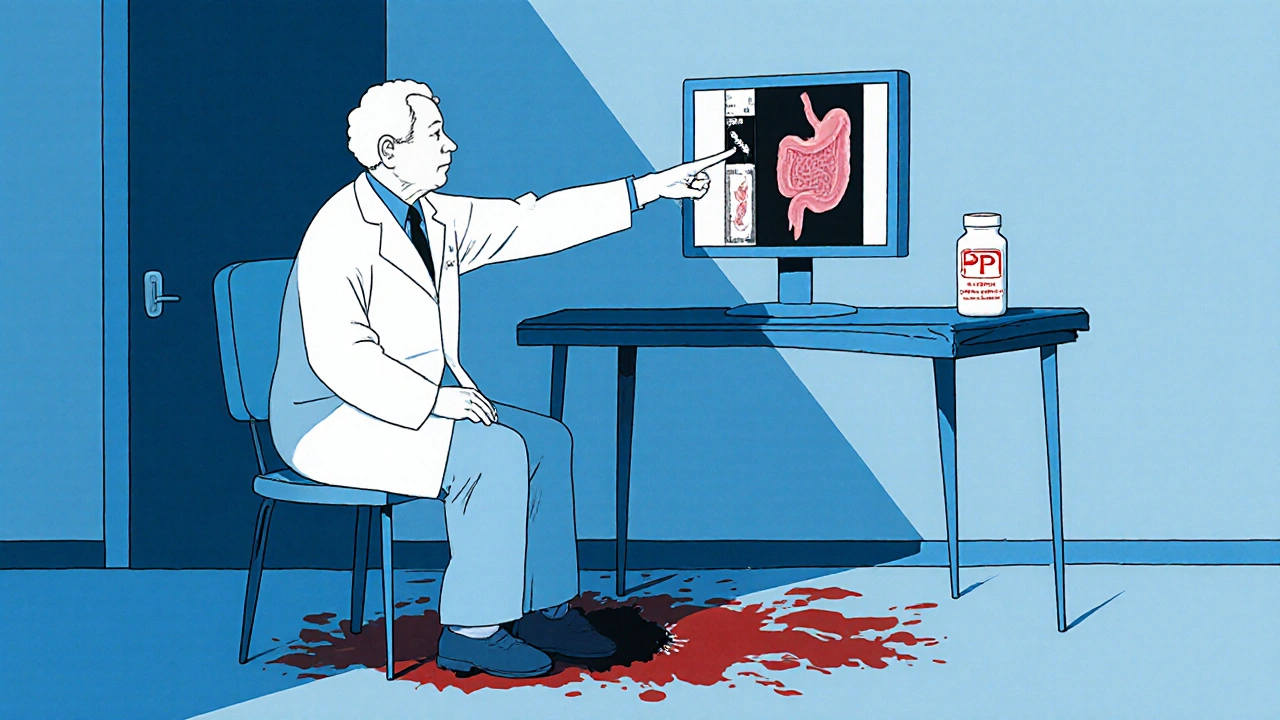
NSAID Overdose: How to Spot and Prevent Gastrointestinal Bleeding Risks
 Nov, 14 2025
Nov, 14 2025
NSAIDs Are Everywhere-But They’re Not as Safe as You Think
You grab ibuprofen for a headache. Your partner takes naproxen for arthritic knees. Your mom swallows a daily low-dose aspirin to protect her heart. These aren’t rare habits-they’re routine. But here’s the truth most people don’t know: NSAIDs are one of the leading causes of preventable gastrointestinal bleeding in adults over 50.
It doesn’t take a massive overdose. Even taking the right dose, every day, for months can quietly damage your stomach and intestines. You might feel fine. No burning, no nausea. Then one day, you’re dizzy, weak, and your stool turns black. By then, you’ve lost a lot of blood-and you’re in the hospital.
How NSAIDs Actually Hurt Your Gut
NSAIDs-like ibuprofen, naproxen, diclofenac, and aspirin-work by blocking enzymes called COX-1 and COX-2. COX-2 causes pain and swelling. COX-1 protects your stomach lining by making mucus and keeping blood flowing to the gut. When you block COX-1, you’re removing the shield.
That damage doesn’t wait for symptoms. Studies show up to 70% of people who take NSAIDs long-term have visible erosions, ulcers, or bleeding in their stomach or intestines-seen during endoscopy. But only about 10% ever report pain or discomfort. That means most people don’t know they’re bleeding until it’s serious.
This isn’t just about stomach ulcers. NSAIDs can cause bleeding anywhere in the digestive tract: from the esophagus down to the colon. In fact, one study found that over half of NSAID users who became anemic showed no signs of bleeding on endoscopy. The damage was happening in the small intestine, where we don’t usually look.
Who’s at the Highest Risk?
Not everyone is equally at risk. Some people are walking into danger without realizing it.
- People over 65: Age weakens the stomach lining and slows healing. The risk of bleeding doubles after 65.
- Those with past ulcers or bleeding: If you’ve had a stomach bleed before, your chance of another one is five times higher if you take NSAIDs again.
- People on blood thinners: Taking aspirin (even low-dose) with another NSAID? That’s a dangerous combo. Your risk of bleeding jumps two to four times. Add in clopidogrel or warfarin? The numbers get worse.
- Those with H. pylori infection: This common stomach bacteria makes NSAID damage worse. It doesn’t cause bleeding on its own-but with NSAIDs, it pushes you over the edge.
- People taking multiple NSAIDs: Mixing prescription and over-the-counter versions (like Advil and a prescription naproxen) is a common mistake. It doesn’t make pain better-it just makes bleeding more likely.
Here’s the scary part: over a third of people admitted for GI bleeding were using over-the-counter aspirin daily-thinking it was harmless. Many didn’t even tell their doctor.
Aspirin Isn’t Safe Just Because It’s Low-Dose
Doctors tell patients to take 81 mg of aspirin daily to prevent heart attacks. That’s good advice-for some. But here’s what they don’t always say: even that tiny dose increases your risk of stomach bleeding by two to four times.
And increasing the dose doesn’t help your heart any more. Taking 150 mg or 300 mg of aspirin doesn’t lower your heart attack risk further-but it does raise your bleeding risk. Odds of bleeding? 2.3 for 75 mg, 3.2 for 150 mg, 3.9 for 300 mg.
Enteric-coated or buffered aspirin? Doesn’t help. Studies prove it. The coating doesn’t stop the drug from damaging your gut lining. It just delays it slightly.
And if you’re on aspirin for your heart and also take ibuprofen for arthritis? You’re not just doubling your risk-you’re creating a perfect storm. The combination increases the chance of both GI bleeding and heart events like stroke or another heart attack.
What You Can Do to Protect Yourself
NSAIDs aren’t evil. They help millions. But they need to be used like a scalpel-not a hammer.
- Ask yourself: Do I really need this? Can you manage pain with heat, rest, physical therapy, or acetaminophen? Acetaminophen doesn’t harm your stomach like NSAIDs do.
- Use the lowest dose for the shortest time. If you’re taking NSAIDs daily for more than a few weeks, you’re in high-risk territory.
- Never mix NSAIDs. Don’t take ibuprofen if you’re already on naproxen. Don’t take Advil if you’re on aspirin. Read labels-many cold and flu meds contain NSAIDs.
- Talk to your doctor before starting daily aspirin. If you’re over 60, have a history of ulcers, or take other meds, aspirin might do more harm than good.
- If you’re on aspirin for heart protection and need pain relief, ask about alternatives. Acetaminophen is safer. In some cases, your doctor may prescribe a COX-2 inhibitor like celecoxib-but even that isn’t risk-free, especially if you’re also on aspirin.
And if you’re already on a PPI (like omeprazole) to protect your stomach? That helps-mostly with the upper GI tract. But it won’t stop bleeding in your small intestine. So it’s not a free pass to keep taking NSAIDs long-term.
Signs You Might Be Bleeding (Even If You Feel Fine)
Don’t wait for black stools or vomiting blood. By then, you’re already in crisis.
- Unexplained fatigue or weakness
- Dizziness or lightheadedness when standing
- Pale skin or cold hands
- Shortness of breath with light activity
- Iron deficiency anemia with no other cause
- Dark, tarry, or sticky stools (melena)
- Bright red blood in stool (could mean lower GI bleeding)
Iron deficiency anemia is often the first clue. If your blood test shows low iron and you’re on NSAIDs-even if you feel fine-ask your doctor to check for hidden GI bleeding.
What Happens If You Overdose?
An NSAID overdose isn’t like an opioid overdose. You won’t stop breathing. But you can still die from it.
Large doses cause severe damage to the stomach and intestinal lining, leading to rapid bleeding, perforation, or kidney failure. Symptoms include vomiting (sometimes with blood), severe abdominal pain, confusion, rapid heartbeat, and fainting.
If someone takes a massive overdose-say, 20 ibuprofen tablets at once-get them to the ER immediately. Treatment includes activated charcoal (if caught early), IV fluids, blood transfusions, and sometimes surgery.
But here’s the real danger: most overdose cases aren’t accidental. They’re the result of long-term misuse. People think, “I’ve been taking this for years, so more can’t hurt.” That’s how emergencies happen.

What Doctors Should Be Doing
Guidelines from the American College of Cardiology and the American Gastroenterological Association say this clearly: before prescribing any NSAID, doctors must assess your risk.
That means asking:
- Have you ever had a stomach ulcer or bleed?
- Are you over 65?
- Are you on aspirin, clopidogrel, or warfarin?
- Do you have kidney disease or heart failure?
- Are you taking more than one NSAID?
If any of these apply, they should offer gastroprotection-usually a proton pump inhibitor (PPI). But even then, they should consider whether the NSAID is even necessary.
Too often, doctors just write the prescription and move on. Patients don’t get the full picture. That’s why so many end up in the ER.
The Bottom Line: NSAIDs Are Not Harmless
They’re powerful tools. But they’re not candy. Every pill you take has a cost.
If you’re on NSAIDs daily, especially if you’re over 50 or on aspirin, talk to your doctor. Ask: Is this still the best option? Are there safer alternatives? Should I be on a stomach protector? Could I cut back?
And if you’re taking over-the-counter NSAIDs without a prescription, stop assuming they’re safe. Millions of people are quietly bleeding because they thought a painkiller couldn’t hurt them.
Know your risk. Protect your gut. Your life might depend on it.
Can I take ibuprofen if I’m on low-dose aspirin for my heart?
It’s not recommended. Taking ibuprofen with low-dose aspirin increases your risk of gastrointestinal bleeding two to four times. It also reduces aspirin’s ability to protect your heart. If you need pain relief while on aspirin, use acetaminophen instead. If you must take ibuprofen, do it only occasionally and talk to your doctor first.
Do enteric-coated NSAIDs prevent stomach bleeding?
No. Enteric-coated or buffered NSAIDs, including aspirin, don’t reduce the risk of bleeding. The coating delays when the drug is released, but it still damages the stomach and intestinal lining. Studies show no meaningful difference in bleeding rates between coated and regular forms.
I feel fine on NSAIDs-do I still need to worry?
Yes. Up to 70% of people on long-term NSAIDs have visible damage in their gut, but only 10% have symptoms. Bleeding can happen without pain, nausea, or warning. The first sign might be fatigue, dizziness, or low iron levels from hidden blood loss. If you’ve been taking NSAIDs daily for months, ask your doctor for a blood test and consider a GI risk assessment.
What’s the safest painkiller for someone with a history of stomach ulcers?
Acetaminophen (paracetamol) is the safest choice for pain relief if you have a history of ulcers or GI bleeding. It doesn’t affect the stomach lining like NSAIDs do. Avoid all NSAIDs-including aspirin-unless your doctor prescribes them with a strong stomach-protecting medication like a PPI, and even then, only if absolutely necessary.
Can NSAIDs cause bleeding in the lower intestine?
Yes. While most bleeding from NSAIDs happens in the stomach or upper small intestine, they can also damage the colon and lower gut. This can cause bleeding that shows up as bright red blood in stool. It’s harder to diagnose because endoscopies usually don’t reach far enough down. If you have unexplained lower GI bleeding and take NSAIDs regularly, stop them and get tested.
Are COX-2 inhibitors like celecoxib safer than regular NSAIDs?
They may reduce upper GI bleeding risk compared to traditional NSAIDs-but only if you’re not taking aspirin. If you’re on low-dose aspirin, COX-2 inhibitors offer no extra protection and still carry the same bleeding risk. They also carry higher heart risks in some people. They’re not a magic solution-just another option that needs careful review with your doctor.
What to Do Next
If you’re on daily NSAIDs, take these three steps this week:
- Check your medicine cabinet. Are you taking more than one NSAID? Stop the extra ones.
- Look at your blood test results. Is your iron low? Ask your doctor if it could be from hidden GI bleeding.
- Book a quick appointment with your GP. Say: “I’ve been taking NSAIDs regularly. Can we review if I still need them?”
Preventing a GI bleed isn’t about avoiding painkillers entirely. It’s about using them wisely. One conversation with your doctor could save you a hospital stay-or worse.
Jennifer Walton
November 15, 2025 AT 14:47Kihya Beitz
November 16, 2025 AT 14:51Chris Bryan
November 17, 2025 AT 05:46Jonathan Dobey
November 17, 2025 AT 13:30John Foster
November 19, 2025 AT 01:02Edward Ward
November 19, 2025 AT 15:17Andrew Eppich
November 20, 2025 AT 22:26Jessica Chambers
November 22, 2025 AT 12:52Shyamal Spadoni
November 22, 2025 AT 21:47Ogonna Igbo
November 24, 2025 AT 07:43BABA SABKA
November 25, 2025 AT 05:57ASHISH TURAN
November 26, 2025 AT 01:32Ryan Airey
November 27, 2025 AT 01:16Hollis Hollywood
November 28, 2025 AT 20:06