Nephrotic Syndrome: Understanding Heavy Proteinuria, Swelling, and Effective Treatments
 Jan, 24 2026
Jan, 24 2026
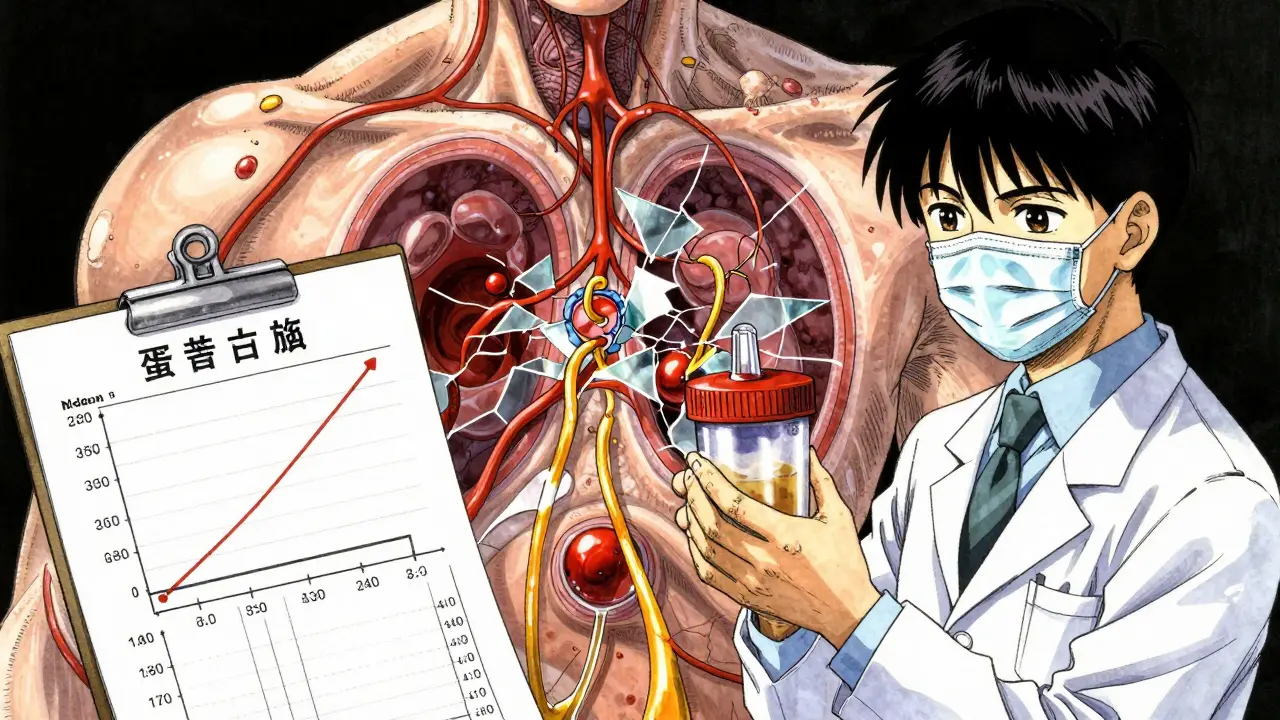
What Is Nephrotic Syndrome?
Nephrotic syndrome is a kidney disorder marked by massive protein loss in urine, low blood protein levels, severe swelling, and high cholesterol. It’s not a disease on its own-it’s a sign that something’s wrong with the filtering units of your kidneys, called glomeruli. These tiny filters normally keep proteins like albumin in your blood. When they get damaged, proteins leak out, pulling water with them into tissues. That’s why swelling shows up around the eyes, ankles, or belly.
Adults typically lose more than 3.5 grams of protein in a 24-hour urine sample. Kids are measured differently-over 40 mg per square meter of body surface area per hour. Blood albumin drops below 3.0 g/dL in adults and often below 2.5 g/dL in children. Cholesterol levels frequently climb above 300 mg/dL. These four signs-proteinuria, hypoalbuminemia, edema, and hyperlipidemia-are the classic hallmarks.
Why Does Protein Leak Out?
The real culprit is damage to the glomerular filtration barrier. This barrier has three layers: the capillary walls, a basement membrane, and specialized cells called podocytes. Podocytes have foot-like projections that wrap around capillaries and connect via a delicate structure called the slit diaphragm. Proteins like nephrin and podocin hold this structure together.
When these proteins are mutated-as in rare genetic forms like congenital nephrotic syndrome-or when the immune system attacks them, the slit diaphragm breaks down. It’s like a sieve with holes too big for the job. Albumin and other proteins slip through, ending up in the urine. This triggers the body to produce more cholesterol and retain fluid, leading to the full picture of nephrotic syndrome.
Heavy Proteinuria: The First Red Flag
For many people, foamy or bubbly urine is the first symptom they notice. It’s not just a coincidence-it’s protein. In fact, 65% of adults with nephrotic syndrome report foamy urine before any swelling appears. In children, parents often mistake the puffiness around the eyes for allergies or lack of sleep.
That swelling? It’s called edema. It starts subtly-maybe puffy eyes in the morning-and can grow to massive proportions. Some adults gain 10 to 15 pounds in days from fluid alone. Fluid can collect in the abdomen (ascites) or lungs (pleural effusion), making breathing hard. In severe cases, people can’t tie their shoes or button their shirts.
Doctors confirm proteinuria with a 24-hour urine collection. A simple dipstick test can hint at it, but only lab measurements give the full picture. A single positive test isn’t enough. You need three consecutive readings of 2+ or higher on a dipstick to call it a relapse. Remission means three straight negative or trace results.
Who Gets Nephrotic Syndrome?
Age matters a lot. In kids, especially between ages 1 and 6, over 80% of cases are caused by minimal change disease. It’s mysterious-under the microscope, the kidneys look almost normal. But it responds well to steroids. In adults, the causes are more varied. Focal segmental glomerulosclerosis (FSGS) accounts for 40% of cases. Membranous nephropathy is next at 30%. Diabetes is responsible for 20-30% of cases in adults over 65.
Secondary causes include lupus, hepatitis B or C, and certain drugs like NSAIDs or penicillamine. Genetic forms are rare-less than 1%-but they hit hard. Congenital nephrotic syndrome, caused by NPHS1 gene mutations, shows up in the first 3 months of life with protein loss over 10 grams per day. These babies need specialized care from day one.
Nephrotic vs. Nephritic: Don’t Mix Them Up
People often confuse nephrotic syndrome with nephritic syndrome. They’re opposites. Nephrotic means lots of protein, low albumin, swelling, and high cholesterol. Nephritic means blood in the urine (hematuria), high blood pressure, reduced kidney function, and red blood cell casts in the urine. Nephritic syndrome usually comes from inflammation like glomerulonephritis. Nephrotic comes from a leaky filter. The treatment paths are totally different.
How Is It Treated?
First-line treatment for children with minimal change disease is prednisone. Most respond within 4 weeks. The dose is 60 mg per square meter of body surface area (up to 80 mg daily) for 4 to 6 weeks, then slowly tapered over 2 to 5 months. In adults, the dose is 1 mg per kg per day (also capped at 80 mg) for 8 to 16 weeks.
Success rates? About 80-90% of kids go into remission. But relapses are common-60-70% of them happen at least once. Viral infections like colds or flu often trigger them. Adults respond less reliably-only 60-70% achieve remission-and half of them relapse.
For those who don’t respond to steroids, or relapse too often, doctors turn to other drugs. Calcineurin inhibitors like tacrolimus or cyclosporine are common next steps. Rituximab, a monoclonal antibody, is increasingly used in both children and adults. Newer drugs like sparsentan (a dual endothelin/angiotensin blocker) have shown 47.6% reduction in proteinuria in clinical trials-much better than older options.
Medications That Protect the Kidneys
Regardless of the cause, ACE inhibitors (like lisinopril) or ARBs (like losartan) are recommended for everyone with nephrotic syndrome. They don’t just lower blood pressure-they directly reduce protein leakage. Studies show they cut proteinuria by 30-50%. The goal? Blood pressure below 130/80 mmHg.
And yes, cholesterol matters too. Statins are often prescribed. High cholesterol isn’t just a number-it increases heart disease risk, which is already elevated in nephrotic syndrome.
Diet and Lifestyle: What You Can Do
Diet plays a huge role. Sodium restriction is critical. Cutting salt to under 2,000 mg per day can reduce swelling by 30-50% in just 72 hours. Avoid processed foods, canned soups, and fast food-they’re loaded with hidden salt.
Protein intake? Don’t overdo it. Eating too much protein can make your kidneys work harder. Stick to 0.8-1.0 grams per kilogram of body weight daily. That’s about 50-70 grams for most adults. Too little can cause muscle loss, too much can worsen proteinuria.
Fluid intake usually doesn’t need to be restricted unless swelling is extreme. But monitoring daily weight helps catch fluid retention early. A 2-pound gain in a day is a red flag.
Big Risks You Can’t Ignore
Nephrotic syndrome isn’t just about swelling and protein. It raises your risk of blood clots-by 2 to 4 times. Renal vein thrombosis (a clot in the kidney’s main vein) happens in 10-40% of adults with albumin below 2.0 g/dL. That’s why some patients need blood thinners like warfarin or low-molecular-weight heparin.
Infection risk is also higher. The immune system gets weakened by both the disease and the steroids. Always check vaccination status before starting treatment. Live vaccines (like MMR or chickenpox) are dangerous during steroid therapy. Inactivated shots (flu, pneumonia, COVID) are safe and recommended.
Monitoring Progress
Weekly urine dipstick tests are standard during active disease. They’re cheap, quick, and tell you if you’re in remission or relapsing. Blood tests for albumin, cholesterol, and kidney function (creatinine, eGFR) are done every 2-4 weeks.
For kids, growth charts matter. Steroids can stunt growth if used too long. Doctors watch height and weight closely. For adults, heart health is tracked-blood pressure, lipid panels, and EKGs may be needed.
What’s New in Treatment?
Research is moving fast. In 2023, the FDA approved budesonide (Tarpeyo) for IgA nephropathy-and it’s showing promise in some FSGS cases, cutting proteinuria by 31-59%. The NEPTUNE study identified three molecular subtypes of FSGS, which could soon help doctors pick the right drug for the right patient.
Drugs targeting the podocyte’s actin cytoskeleton-like Rho kinase inhibitors-are in early trials. In animal models, they reduce proteinuria by 60-70%. That’s huge. Precision medicine is coming to nephrotic syndrome.
Prognosis: What’s the Long-Term Outlook?
It depends on the cause. Minimal change disease has a 95% 10-year kidney survival rate. FSGS? Only 50-70%. Membranous nephropathy is in the middle at 60-80%. But if you have diabetes-related nephrotic syndrome, your 10-year survival drops to 40-50%.
The biggest warning sign? Persistent proteinuria over 1 gram per day after treatment. That increases your risk of kidney failure by 4.2 times. That’s why getting to complete remission isn’t optional-it’s life-saving.
Real Stories, Real Challenges
Parents on patient forums often say their child was misdiagnosed for 7-10 days because the swelling looked like allergies. Adults describe gaining 15 pounds in a week and thinking they’d just gained weight. Steroid side effects are brutal: moon face, ravenous hunger, mood swings. One mom said her 6-year-old went from sweet to angry overnight. It’s not just physical-it’s emotional.
But there’s hope. At Children’s Hospital of Philadelphia, 85% of kids with minimal change disease achieve full remission with steroids. Even with relapses, most grow up with normal kidney function.
When to See a Specialist
If you or your child has persistent swelling, foamy urine, or unexplained weight gain, don’t wait. Start with your doctor. If proteinuria is confirmed, ask for a nephrologist referral. A kidney biopsy may be needed-especially in adults or if steroids don’t work.
Early diagnosis saves kidneys. Early treatment saves lives.
Is nephrotic syndrome curable?
It depends on the cause. Minimal change disease often goes into long-term remission with treatment, especially in children. Many kids outgrow it. But diseases like FSGS or diabetic nephropathy are chronic. The goal isn’t always a cure-it’s controlling protein loss, protecting kidney function, and preventing complications.
Can nephrotic syndrome come back after treatment?
Yes, relapses are common. About 60-70% of children with minimal change disease have at least one relapse, often after a cold or virus. Adults have even higher relapse rates. That’s why ongoing monitoring and quick action at the first sign of swelling or foamy urine are so important.
Are steroids the only treatment option?
No. Steroids are first-line for many, especially children. But if they don’t work, or if side effects are too severe, doctors use other drugs like calcineurin inhibitors (tacrolimus, cyclosporine), rituximab, or newer agents like sparsentan. The choice depends on age, cause, and response history.
Does diet really make a difference?
Absolutely. Reducing sodium to under 2,000 mg per day can cut swelling by half in just a few days. Eating the right amount of protein-neither too much nor too little-helps protect the kidneys. No diet cures it, but poor diet makes it worse.
Can I get vaccinated while on treatment?
Inactivated vaccines like flu, pneumonia, and COVID shots are safe and strongly recommended. Live vaccines-like MMR or chickenpox-are dangerous during steroid or immunosuppressant therapy. Always check with your nephrologist before getting any shot.
What’s the biggest danger of nephrotic syndrome?
The biggest danger is not the swelling-it’s the long-term kidney damage from ongoing protein loss. Persistent proteinuria over 1 gram per day increases your risk of kidney failure by more than four times. That’s why achieving complete remission matters more than just feeling better.
Shelby Marcel
January 24, 2026 AT 23:41