Monitoring Your Health After Switching to Generics
 Dec, 10 2025
Dec, 10 2025
Switching from a brand-name drug to a generic version is one of the most common changes in your medication routine-and it’s usually completely safe. In fact, generic medications make up over 90% of all prescriptions filled in the U.S., and they save patients and the healthcare system billions every year. But even though generics are required by law to work the same way as their brand-name counterparts, some people notice subtle changes after making the switch. That’s why monitoring your health after switching to generics isn’t just a good idea-it’s necessary for certain medications.
Why You Might Notice a Difference
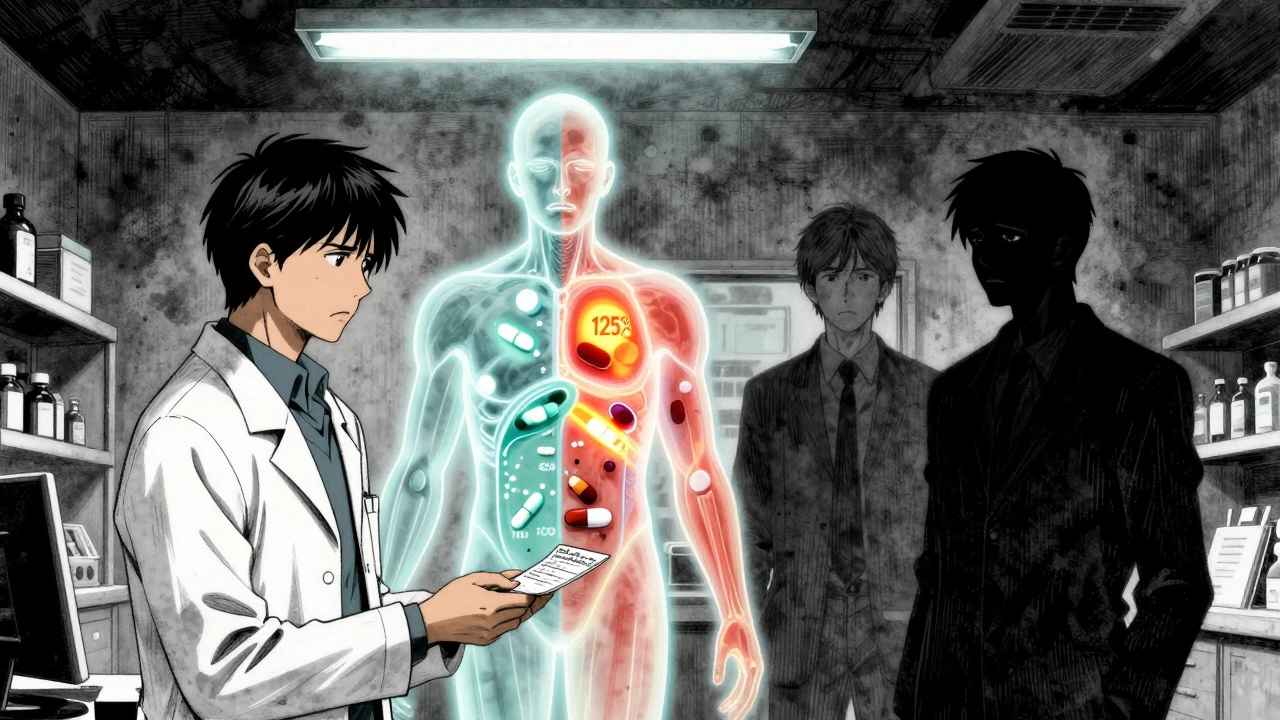
The FDA requires generic drugs to have the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also prove they deliver the same amount of medicine into your bloodstream at the same rate. This is called bioequivalence. To pass, the generic’s absorption must fall within 80-125% of the brand-name drug’s levels. That’s a wide enough range to account for normal biological variation, but not so wide that it compromises safety. Still, that 80-125% window means there’s room for small differences in how quickly or completely your body absorbs the drug. For most people, this doesn’t matter. But for those taking medications with a narrow therapeutic index-where the difference between an effective dose and a toxic one is very small-even a small change can cause problems. Drugs like warfarin (a blood thinner), levothyroxine (for thyroid conditions), and certain anti-seizure medications like lamotrigine fall into this category. If your body absorbs slightly less of the drug, your condition could flare up. If it absorbs slightly more, you could experience side effects. That’s why monitoring isn’t about doubting generics-it’s about making sure your body responds the same way.Which Medications Need Extra Attention
Not all generics need close monitoring. But if you’re taking any of these, pay extra attention for the first 30 to 90 days after switching:- Levothyroxine - Used for hypothyroidism. Even small changes in absorption can affect your energy, weight, heart rate, and mood. Studies show about 12% of people switching to a different generic report symptoms like fatigue or palpitations.
- Warfarin - A blood thinner. Your INR (blood clotting time) must stay in a tight range. A shift in absorption can increase your risk of bleeding or clotting.
- Lamotrigine, phenytoin, carbamazepine - Anti-seizure drugs. A small drop in blood levels can trigger breakthrough seizures.
- Bupropion - An antidepressant and smoking cessation aid. Some users report changes in mood, sleep, or anxiety after switching generics.
- Cyclosporine, tacrolimus - Immunosuppressants used after organ transplants. These require strict blood level monitoring regardless of brand or generic, but switching can still cause fluctuations.
How to Monitor Your Health After Switching
You don’t need to be a doctor to track your health. Here’s how to do it simply and effectively:- Keep a daily log - For at least 30 days after switching, write down how you feel. Note things like energy levels, sleep quality, mood swings, dizziness, headaches, or unusual symptoms. Use a notebook, phone app, or even a sticky note on your fridge.
- Track key biomarkers - If you’re on thyroid medication, check your TSH levels at 4 and 8 weeks after switching. If you’re on warfarin, get your INR checked at 7-14 days and again at 30 days. Diabetics should check HbA1c at 4 and 8 weeks. People with epilepsy should track seizure frequency.
- Watch for side effects - New or worsening nausea, rash, dizziness, or mood changes could signal a reaction. Don’t assume it’s “just stress.”
- Check the pill - Generics look different. If your pill suddenly changes color, shape, or size, that’s normal-but only if it’s from the same manufacturer. If you get a different generic from a different company, that’s a new switch. Ask your pharmacist to confirm the manufacturer and NDC code.
What to Do If You Notice a Problem
If you feel worse after switching, don’t just power through. Here’s what to do:- Don’t stop taking the medication - Stopping suddenly could be dangerous, especially with blood thinners or seizure meds.
- Contact your doctor - Tell them exactly when you switched, what you’re feeling, and what changes you’ve noticed. Bring your medication log.
- Ask for a lab test - If your condition is monitored with blood tests (like INR, TSH, or drug levels), request one immediately.
- Request your original generic - If you were doing fine on one generic brand, ask your pharmacist to stick with that one. Not all generics are made the same, even if they contain the same active ingredient.
How to Avoid Unnecessary Switches
Pharmacies often switch generics automatically to save money. But you have rights:- Ask for the brand or a specific generic - If you’ve had good results with one, ask your doctor to write “Dispense as Written” or “Do Not Substitute” on the prescription.
- Know your NDC number - Every drug has a unique 10-digit National Drug Code. Write it down when you get your prescription. If it changes next refill, ask why.
- Use the FDA’s Orange Book - It lists which generics are rated as therapeutically equivalent. Look up your drug to see if any are flagged for potential issues.
Real Stories, Real Results
A 68-year-old woman in Dunedin switched from brand-name levothyroxine to a generic and noticed her heart racing and hands shaking within a week. Her TSH level jumped from 2.1 to 6.8-clearly undermedicated. After switching back to her original generic, her levels normalized in two weeks. Another man with epilepsy had been seizure-free for five years on a specific generic lamotrigine. After a pharmacy switch, he had two seizures in 10 days. His neurologist confirmed his blood levels had dropped. He requested the original manufacturer-and hasn’t had another seizure since. These aren’t rare cases. They’re why monitoring matters.
When You Can Relax
The good news? For most people, switching to generics is seamless. If you’re taking statins, blood pressure meds like lisinopril, or antibiotics like amoxicillin, you’re unlikely to notice a difference. Studies show over 90% of patients report no change in symptoms or side effects after switching. The key is knowing your medication class. If your drug isn’t on the narrow therapeutic index list, you can switch with confidence. Still, keeping an eye on how you feel for the first few weeks is smart-just in case.Reporting Problems Helps Everyone
If you experience a real problem after switching to a generic, report it. The FDA’s MedWatch program collects reports from patients and doctors to spot safety trends. In 2022, over 1.2 million reports were filed-but only a small fraction were about generics. Most go unreported. You don’t need to be an expert. Just tell them:- What drug you took (brand and generic name)
- The lot number and NDC code from the bottle
- When you switched
- What symptoms you had
- Whether you went back to the original
Final Thoughts
Generic medications are safe, effective, and save money. But safety doesn’t mean “one size fits all.” Your body reacts to subtle differences in how a drug is made-even if the active ingredient is identical. Monitoring your health after switching to generics isn’t about fear. It’s about control. It’s about knowing your body well enough to recognize when something’s off. If you’re on a high-risk medication, track your symptoms. Talk to your doctor. Know your NDC. Don’t assume all generics are the same. And if something feels wrong-trust yourself. You’re the best monitor of your own health.Are generic medications really as effective as brand-name drugs?
Yes, for the vast majority of people, generic medications are just as effective. The FDA requires them to meet the same standards for safety, strength, purity, and performance as brand-name drugs. They must prove bioequivalence-meaning they deliver the same amount of active ingredient into your bloodstream at the same rate. Over 90% of prescriptions in the U.S. are generics, and studies show they work just as well for most conditions.
Why do some people feel worse after switching to generics?
Some people, especially those taking drugs with a narrow therapeutic index (like warfarin, levothyroxine, or anti-seizure meds), may notice small differences in how their body absorbs the medication. Generics can have different inactive ingredients (fillers, dyes, coatings), which can affect how quickly the drug dissolves. For most, this doesn’t matter-but for a small group, even a slight change can cause symptoms like fatigue, mood shifts, or breakthrough seizures.
Which generic medications need the most monitoring?
The medications that need closest monitoring are those with a narrow therapeutic index: levothyroxine (thyroid), warfarin (blood thinner), lamotrigine and phenytoin (anti-seizure), bupropion (antidepressant), and immunosuppressants like cyclosporine. These drugs require precise blood levels, and even small changes in absorption can lead to serious side effects or loss of effectiveness.
How long should I monitor my health after switching to a generic?
For most people, monitor for at least 30 days. If you’re on a high-risk medication like levothyroxine or warfarin, monitor for 60-90 days and get lab tests at 7-14 days and again at 30 days. Your doctor may recommend more frequent checks based on your condition and medication.
Can I ask my pharmacist to stick with the same generic brand?
Yes. You can ask your doctor to write “Dispense as Written” or “Do Not Substitute” on your prescription. You can also ask your pharmacist which generic manufacturer you’re getting and request the same one each time. The NDC code on the bottle tells you exactly which company made it. If it changes, ask why.
What should I do if I think my generic isn’t working?
Don’t stop taking it. Contact your doctor immediately. Bring your medication log and the pill bottle. Ask for a blood test if your condition is monitored that way (like INR for warfarin or TSH for thyroid meds). If symptoms started after the switch, your doctor may switch you back to your original generic or brand-name version. Report the issue to the FDA’s MedWatch program to help others.
Is it safe to switch back and forth between generics?
It’s not recommended, especially for drugs with narrow therapeutic indices. Each time you switch manufacturers, even if both are generics, you’re introducing a new formulation. This can cause fluctuations in how your body absorbs the drug. Stick with one manufacturer if you’re doing well. If your pharmacy keeps switching, ask your doctor to write “Do Not Substitute.”
Monica Evan
December 11, 2025 AT 00:56Jim Irish
December 12, 2025 AT 16:52Eddie Bennett
December 14, 2025 AT 13:42Sylvia Frenzel
December 16, 2025 AT 12:50Doris Lee
December 17, 2025 AT 02:58Michaux Hyatt
December 18, 2025 AT 09:26Raj Rsvpraj
December 19, 2025 AT 17:46Jack Appleby
December 21, 2025 AT 09:56Frank Nouwens
December 21, 2025 AT 12:09Aileen Ferris
December 22, 2025 AT 01:27Michelle Edwards
December 23, 2025 AT 05:28Sarah Clifford
December 24, 2025 AT 05:13Regan Mears
December 24, 2025 AT 07:08