Medication Side Effects in Elderly Patients: Why Age Changes Everything
 Jan, 8 2026
Jan, 8 2026
Beers Criteria Medication Checker
Medication Safety Check for Seniors
The Beers Criteria is the gold standard for identifying medications that may be inappropriate for older adults due to increased risk of side effects. Check if your medication might be on the list.
When you’re 70, a pill that helped you at 50 might make you dizzy, confused, or fall down. It’s not your imagination. Your body doesn’t process medicine the same way it used to. And that’s why medication side effects in elderly patients are so dangerous - and so common.
Why Older Bodies React Differently to Medicines
Your liver and kidneys don’t work as fast after 65. Blood flow to the liver drops by 30-40% between ages 25 and 75. Kidneys filter less each year - about 0.8 mL per minute per 1.73m² after 40. That means drugs stick around longer. A sedative like diazepam might last 24 hours in a 30-year-old. In someone 75? It can hang around for days. That’s why so many older adults feel groggy, unsteady, or foggy even after taking a normal dose.Body fat goes up. Muscle goes down. By age 70, body fat can be 35-40% - up from 25% at 30. Fat-soluble drugs like antidepressants or anti-anxiety meds get trapped in fat tissue. They don’t get cleared out. So even small doses build up. That’s why some seniors on low-dose benzodiazepines end up in the ER after a fall.
The Real Danger: Too Many Pills
Most seniors aren’t on one medication. They’re on five, six, ten. Polypharmacy - taking five or more drugs at once - isn’t just common. It’s the norm. And each extra pill adds risk. Not because the drugs are bad. But because they interact.Take NSAIDs like ibuprofen. They’re fine alone. But add them to blood thinners like warfarin? Risk of a bleeding stomach ulcer jumps 15 times. Add steroids? Even worse. One study found nearly half of hospital stays for older adults due to side effects were preventable. That’s not bad luck. That’s system failure.
Some combinations are quietly deadly. Corticosteroids plus NSAIDs. SSRIs plus NSAIDs. Anticholinergics plus heart meds. These aren’t rare. They’re routine. And doctors often don’t see the full picture. A cardiologist prescribes one thing. A rheumatologist prescribes another. A pain specialist adds a third. No one looks at the whole list.
Side Effects That Don’t Look Like Side Effects
Younger people get stomach upset or rashes. Seniors? They get falls. Or confusion. Or memory loss. Or sudden weight loss. These aren’t normal aging. They’re red flags.One in five to three in ten falls in older adults are caused by medications. That’s not just a stumble. It’s a broken hip. A hospital stay. A loss of independence. And often, the culprit is something simple: a blood pressure pill that drops pressure too fast. A sleep aid that lingers. An antibiotic that messes with gut bacteria and causes diarrhea - leading to dehydration and dizziness.
Confusion? Could be an antihistamine in an allergy pill. Memory problems? Could be an anticholinergic in an over-the-counter sleep aid. Weight loss? Could be a diuretic that’s too strong. These aren’t symptoms of dementia. They’re symptoms of a drug list that needs a reset.
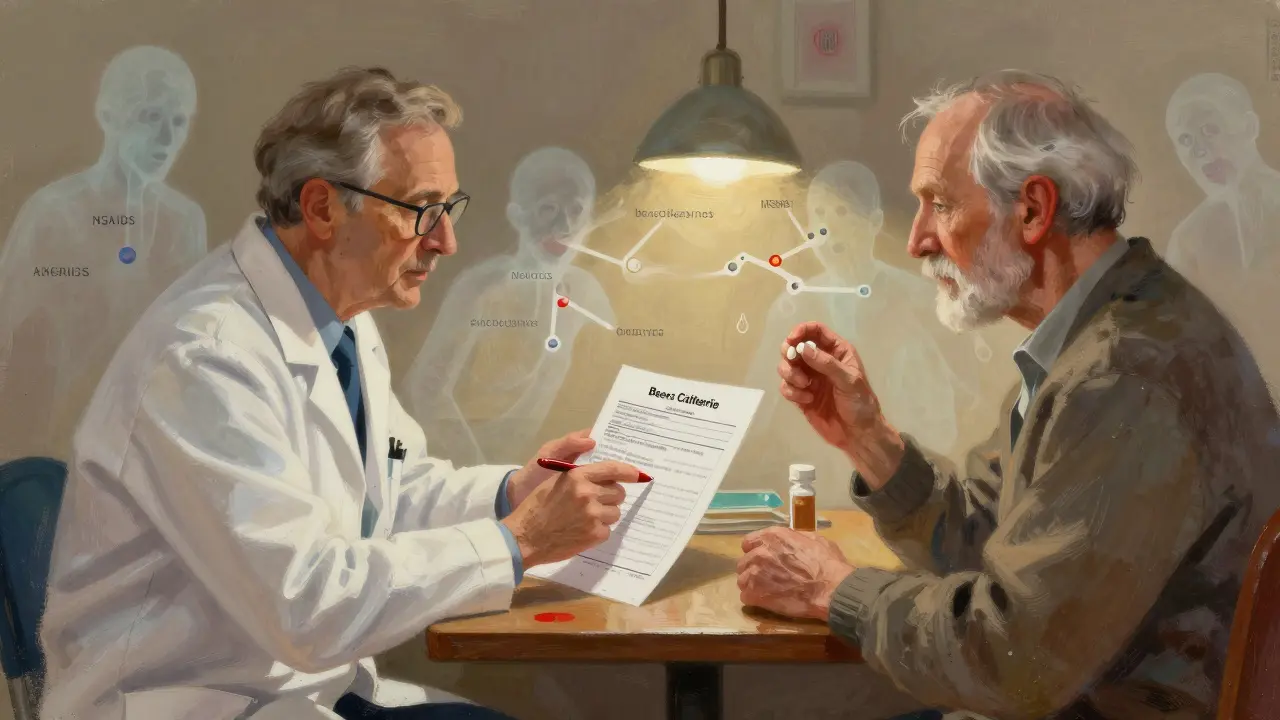
The Beers Criteria: A Lifesaving List
In 1991, Dr. Mark Beers published a list of medications that were risky for older adults. It was simple: avoid these drugs in seniors unless absolutely necessary. Today, it’s updated every few years. The 2023 version is the gold standard.It tells you which drugs to avoid: glyburide (too much risk of low blood sugar), megestrol (can cause blood clots), indomethacin (highest chance of brain fog among NSAIDs), and pentazocine (can cause hallucinations). It warns against sliding-scale insulin - a dangerous way to manage diabetes in frail seniors. It says avoid acetylcholinesterase inhibitors if someone has slow heart rhythms.
But here’s the catch: the Beers Criteria aren’t a rulebook. They’re a conversation starter. A 78-year-old with severe arthritis might need an NSAID. A 90-year-old with dementia might need a low-dose antipsychotic. The list doesn’t say never. It says: think twice.
Doctors who use it don’t just check boxes. They ask: Is this drug still needed? Can we lower the dose? Is there a safer alternative? That’s how you avoid harm without losing benefit.
What Medications Are Most Risky?
Some drugs are just too dangerous for older bodies. Here’s what the experts say to watch for:- Propoxyphene - Outdated painkiller. Less effective than acetaminophen. Higher risk of confusion and heart rhythm problems.
- Phenylbutazone - Rarely used now, but still in some older prescriptions. Can wipe out white blood cells.
- Anticholinergics - Found in many OTC sleep aids, allergies, and bladder meds. Cause dry mouth, constipation, confusion, and memory loss. Even low doses add up.
- Long-acting benzodiazepines - Like diazepam or clonazepam. Stay in the body too long. Increase fall risk by 40-60%.
- NSAIDs - Even ibuprofen and naproxen. Increase risk of stomach bleeding, kidney damage, and heart failure.
And don’t forget supplements. Ginkgo biloba? Can thin blood. St. John’s wort? Interacts with 60+ medications. Elderly patients often don’t tell their doctors about these. They think, “It’s natural, so it’s safe.”
How to Protect Yourself or a Loved One
The solution isn’t stopping all meds. It’s smarter use.- Keep a full list. Write down every pill, patch, cream, vitamin, herb, and supplement. Include dosages and why you’re taking them. Update it every time a new doctor sees you.
- Ask the pharmacist. Pharmacists see all your meds at once. Ask: “Are any of these risky for someone my age?” Most offer free med reviews.
- Ask about deprescribing. Say: “Can we try stopping this one? What if we cut the dose in half?” Don’t be afraid to question a drug you’ve been on for years.
- Watch for new symptoms. If you start feeling foggy, dizzy, or off-balance after starting a new med - tell your doctor. Don’t wait. Don’t assume it’s “just getting older.”
- Use one pharmacy. Keeps all your records in one place. Helps catch dangerous interactions.
Who Should Be Involved?
Managing meds in older adults isn’t just the doctor’s job. It takes a team.Pharmacists are your secret weapon. They spot interactions you and your doctor might miss. Nurses help track side effects. Caregivers notice changes in behavior or mobility. And patients? You’re the most important part. You know when you feel different.
Geriatric specialists don’t just treat diseases. They treat people. They ask: “What matters most to you?” Is it walking without pain? Staying independent? Sleeping through the night? Then they match the meds to those goals - not just to lab numbers.
The Bigger Picture: Why This Matters
By 2030, one in five Americans will be over 65. That’s 95 million people. Right now, 10-23% of hospital admissions in older adults are due to bad drug reactions. Half of them could have been avoided.The cost? $3.5 billion a year in the U.S. alone. But the real cost is harder to measure: lost independence, broken hips, nursing home stays, family stress.
This isn’t about cutting corners. It’s about getting it right. Medications save lives - vaccines, blood pressure pills, insulin. But they can also break them. The goal isn’t fewer drugs. It’s better drugs. Right dose. Right time. Right person.
Older adults deserve medicine that fits their body - not one designed for a 30-year-old.
Why do seniors have more side effects from medications than younger people?
As people age, their liver and kidneys process drugs more slowly. Blood flow to the liver drops by 30-40% between ages 25 and 75. Kidney function declines about 0.8 mL/min/1.73m² each year after 40. Body fat increases while muscle mass decreases, causing some drugs to build up in the body. This means medications stay active longer, increasing the chance of side effects like dizziness, confusion, or falls - even at normal doses.
What is the Beers Criteria and why is it important?
The Beers Criteria is a list of medications that are potentially inappropriate for older adults due to high risk of side effects. First published in 1991 and updated regularly by the American Geriatrics Society, it helps doctors avoid drugs like glyburide, indomethacin, and long-acting benzodiazepines that can cause confusion, falls, or kidney damage in seniors. It’s not a strict rule - it’s a tool to start conversations about safer alternatives and dose adjustments.
Can over-the-counter meds be dangerous for elderly people?
Yes. Many OTC drugs contain anticholinergics - found in sleep aids, allergy meds, and stomach remedies - which can cause memory problems, dry mouth, constipation, and confusion in older adults. Even common pain relievers like ibuprofen can raise the risk of stomach bleeding or kidney damage, especially when taken with blood thinners. Always check with a pharmacist before using OTC meds if you’re over 65.
What should I do if I think a medication is causing side effects?
Don’t stop taking it without talking to your doctor. But do report new symptoms like dizziness, confusion, falls, memory loss, or sudden weight changes. Bring your full medication list - including vitamins and supplements - to your next appointment. Ask: “Could this be caused by one of my meds?” and “Is there a safer option?” Many side effects are reversible once the drug is adjusted or stopped.
Is polypharmacy always bad for seniors?
Not always. Some seniors need multiple medications to manage conditions like diabetes, heart disease, or high blood pressure. The problem isn’t the number of pills - it’s whether each one is still necessary, at the right dose, and not interacting dangerously with others. A medication review with a pharmacist or geriatrician can help identify which drugs can be safely reduced or stopped without losing benefits.
How can caregivers help prevent medication problems in older adults?
Caregivers can help by keeping an updated list of all medications, setting up pill organizers, watching for new symptoms like confusion or unsteadiness, and accompanying the senior to doctor visits to ask questions. They can also encourage the use of one pharmacy to avoid dangerous interactions and remind the senior to report side effects - even if they seem minor.
What Comes Next?
The future of senior care isn’t just more drugs. It’s smarter ones. Research is now looking at pharmacogenomics - how your genes affect how you process medicine. That could one day mean tailoring doses based on your DNA. But for now, the best tools we have are simple: a full list of meds, honest conversations with your doctor, and the courage to ask, “Do I still need this?”If you’re caring for an older adult, don’t assume every pill is necessary. Ask. Review. Reconsider. One less pill might mean one more fall avoided. One more day lived safely at home.
Kunal Majumder
January 10, 2026 AT 15:48My dad’s on six meds and just started falling last month. We thought it was aging, but turns out it was that sleepy-time allergy pill he’s been taking for 15 years. Pharmacist caught it in five minutes. Took him off it - no more dizziness. Simple fix, but nobody asked.
Don’t assume it’s ‘just getting older.’ Sometimes it’s just an old pill that outlived its usefulness.
chandra tan
January 12, 2026 AT 10:37In India, grandmas take 10 different ayurvedic powders, plus blood pressure pills, plus diabetes meds, plus random supplements from the market. No one checks interactions. My aunt ended up in the ER after mixing ashwagandha with warfarin. Natural doesn’t mean safe - especially when you’re 78 and your kidneys are running on fumes.
We need more community pharmacists who speak Hindi and Tamil. Not just English-speaking docs in white coats.
Dwayne Dickson
January 13, 2026 AT 00:48It is, regrettably, an incontrovertible fact that the current paradigm of geriatric pharmacotherapy remains woefully undergirded by evidence-based protocols tailored to the physiological realities of advanced age. The Beers Criteria, while commendable in intent, are often treated as advisory rather than imperative - a tragic lapse in clinical stewardship.
One must ask: when polypharmacy becomes the default, is it not a systemic failure of care coordination, rather than a failure of patient compliance? The answer, I submit, is unequivocally yes.
Ted Conerly
January 14, 2026 AT 20:14Listen - I’ve been a nurse for 28 years. I’ve seen this play out a thousand times. A patient comes in with ‘memory problems.’ Turn out it’s the Benadryl they’ve been taking for insomnia since 2003. Or the ibuprofen they pop like candy. No one’s evil. No one’s lazy. But no one’s looking at the whole list.
Ask your pharmacist. Bring your meds in a bag. Say: ‘Help me cut the clutter.’ You’ll be shocked how many of those pills are ghosts from another life.
Faith Edwards
January 16, 2026 AT 03:02It is utterly deplorable that we have allowed the medical-industrial complex to weaponize convenience over cognition. Seniors are being drugged into submission with OTC anticholinergics, marketed as ‘gentle sleep aids’ by corporations who couldn’t care less if you forget your grandchild’s name.
And yet, the average American elder still believes that ‘natural’ equals ‘safe.’ How quaint. How tragically naive. This isn’t aging - it’s pharmaceutical negligence dressed up as compassion.
Saumya Roy Chaudhuri
January 16, 2026 AT 04:45OMG I KNEW THIS WAS A THING. My uncle took that glyburide thing for 10 years and kept fainting at the temple. Doctors kept saying ‘oh you’re just getting weak.’ NO. IT WAS THE DRUG. I YELLED AT HIS CARDIOLOGIST UNTIL THEY SWITCHED HIM. NOW HE’S WALKING AGAIN. DON’T LET THEM GASLIGHT YOU.
EVERYONE OVER 65 NEEDS A MEDS AUDIT. LIKE, RIGHT NOW. I’M TALKING TO MY MOM TOMORROW AND I’M TAKING HER LIST. NO EXCUSES.
anthony martinez
January 16, 2026 AT 16:50Interesting. I wonder how many of these ‘preventable’ hospitalizations are just people not following instructions. Or is it really the doctors’ fault? I mean, if someone takes two NSAIDs and a blood thinner, maybe they’re just not reading labels.
Still, the system could do better. But blame’s complicated.
Mario Bros
January 17, 2026 AT 05:47My grandma’s on 8 meds. I made her a color-coded chart. Red = morning. Blue = night. Green = ‘only if you’re in pain.’ She still forgets. So now I put them in a pill box with a little alarm that beeps. She hates it. But she hasn’t fallen in 6 months.
It’s not fancy. It’s not high-tech. But it works. And yeah, I nag. But I’d rather nag than bury her.
Just ask your pharmacist. They’re the real MVPs.
Jaqueline santos bau
January 18, 2026 AT 15:10Ugh. I can’t believe people still think ‘natural’ is safe. My cousin’s mother took St. John’s Wort with her antidepressant and ended up in the psych ward. And now she’s blaming the doctors. Like, honey, you didn’t tell them you were swallowing herbal tea like it was vitamin water.
And don’t get me started on those ‘elderly wellness’ influencers on TikTok pushing turmeric capsules as cure-alls. It’s not wellness. It’s dangerous nonsense.
Aurora Memo
January 19, 2026 AT 22:04I’ve worked in geriatric care for over 20 years. The most powerful thing families can do? Show up. Bring the list. Ask the questions. Don’t assume the doctor knows everything. They don’t. And it’s not their fault - they’re overwhelmed.
But if you, as the child, sibling, or friend, take 10 minutes to write down every pill, supplement, and cream - you’ve already saved a life.
It’s not about blame. It’s about care.
Christine Milne
January 21, 2026 AT 00:39Let’s be clear: this is a liberal healthcare agenda disguised as patient advocacy. In my father’s day, people took their medicine and didn’t complain. Now we have people demanding ‘medication reviews’ because they’re too lazy to follow a simple regimen.
And this ‘Beers Criteria’? A politically correct list designed to cut costs, not save lives. If your grandma’s on a few pills, that’s because she’s sick - not because someone failed her.
Stop infantilizing seniors. They’re not children. They’re adults who made choices - and they should live with the consequences.