Inflammatory Bowel Disease: Crohn’s Disease vs. Ulcerative Colitis
 Feb, 1 2026
Feb, 1 2026
When you hear "inflammatory bowel disease," it sounds like one thing-but it’s actually two very different conditions hiding under the same label: Crohn’s disease and ulcerative colitis. Both cause chronic gut inflammation, pain, diarrhea, and fatigue. But they don’t behave the same way, respond to the same treatments, or carry the same risks. Getting them mixed up can lead to the wrong treatment-and that can make things worse.
Where the Inflammation Lives
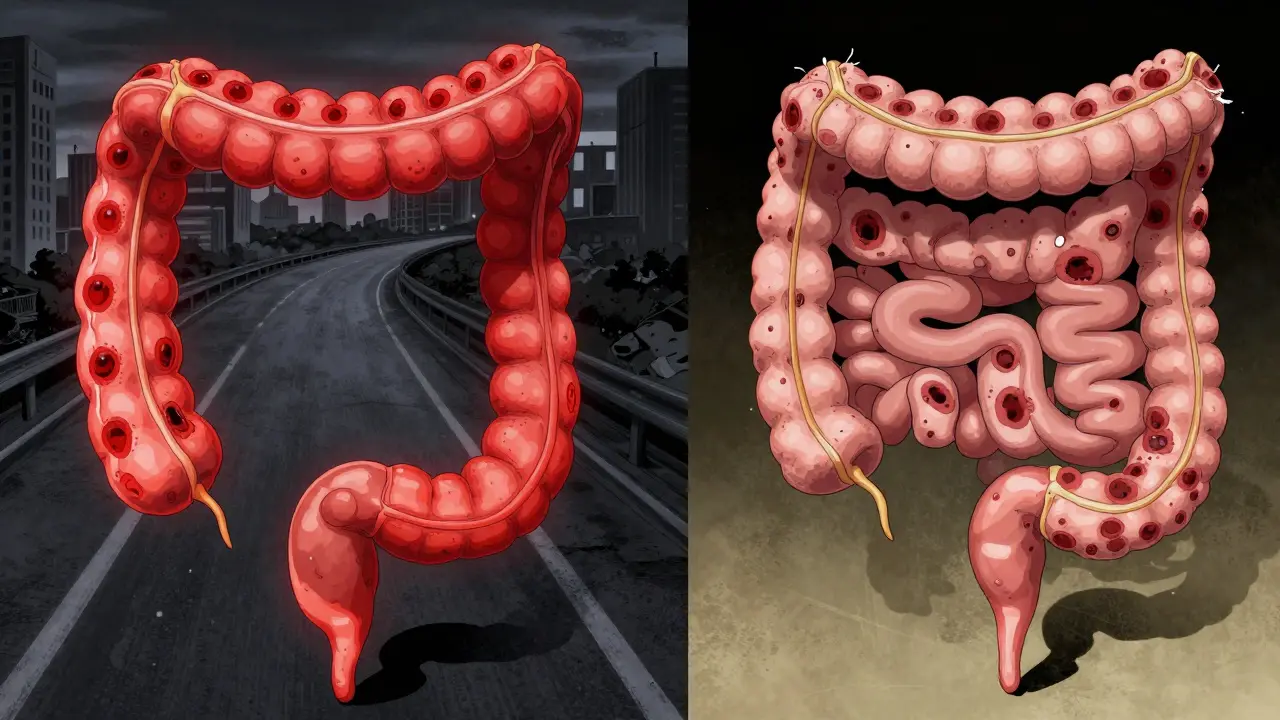
Ulcerative colitis sticks to one place: your colon and rectum. It starts at the very end, in the rectum, and creeps upward in a continuous line. If you have it, your entire colon might be inflamed-or just the lower part. But it never jumps to your small intestine or stomach. Think of it like a slow-burning fire along a straight road. Crohn’s disease doesn’t care about boundaries. It can show up anywhere from your mouth to your anus. Most often, it hits the end of the small intestine (the terminal ileum) and the beginning of the colon. But it can skip around. One patch of intestine is inflamed, then there’s healthy tissue, then another inflamed patch. These are called "skip lesions," and they’re a dead giveaway for Crohn’s. That’s why someone with Crohn’s might have pain near their belly button and also near their rectum-but nothing in between.How Deep Does It Go?
Ulcerative colitis stays shallow. It only eats away at the innermost lining of the colon-the mucosa. That’s why bleeding is so common. The surface is raw, so blood shows up in stool easily. Crohn’s disease goes all the way through. It punches through every layer of the bowel wall: mucosa, submucosa, muscle, even the outer covering. This is called transmural inflammation. And that’s what makes Crohn’s so dangerous long-term. When the whole wall is inflamed, it thickens, narrows, and can scar into strictures. Or worse-it can punch holes through the wall, creating abnormal tunnels called fistulas. These can connect your intestine to your bladder, skin, or even another part of your gut. Fistulas happen in about 25% of people with Crohn’s over time. In ulcerative colitis? Less than 5%.What Happens When Things Go Wrong
Both conditions can flare up, but the complications are different. Ulcerative colitis carries a rare but terrifying risk: toxic megacolon. This is when the colon suddenly balloons out, becomes paralyzed, and can rupture. It’s life-threatening and needs emergency surgery. It happens in about 5% of severe UC cases-but almost never in Crohn’s. Crohn’s disease? It’s more about slow, stubborn damage. Strictures (narrowed sections) affect about one-third of people over time. Many need surgery to cut out the blocked part. But here’s the catch: even after surgery, Crohn’s often comes back right next to the cut. Half of people need another surgery within 10 years. That’s because the disease doesn’t get removed-it just moves on. Ulcerative colitis, on the other hand, can be cured. If your whole colon is destroyed by inflammation, doctors can remove it entirely. Then they build a new internal pouch from your small intestine and attach it to your anus. You still go to the bathroom normally-just more often. That’s not possible with Crohn’s. Removing the bad part doesn’t fix the disease. It just moves to another spot.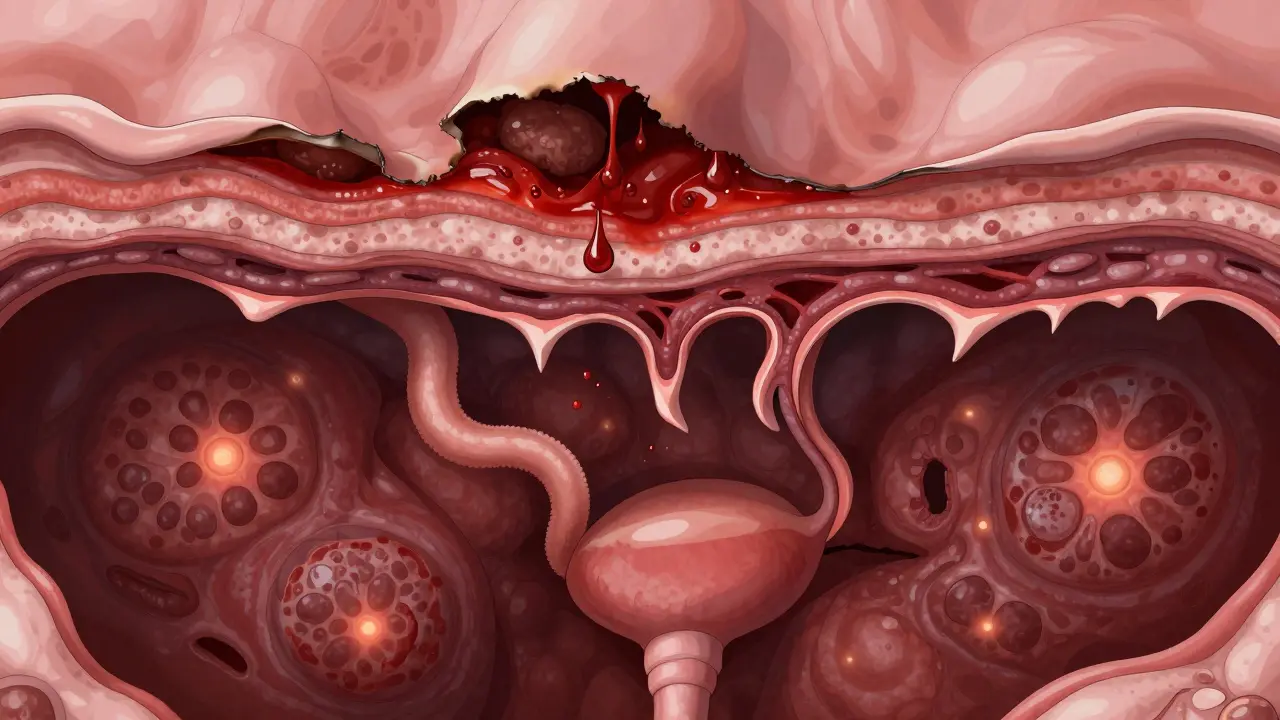
How Doctors Tell Them Apart
There’s no single blood test that says "Crohn’s" or "UC." Diagnosis is like solving a puzzle with four pieces: symptoms, colonoscopy, imaging, and biopsy. During a colonoscopy, if the doctor sees continuous red, raw tissue starting at the rectum, with tiny growths called pseudopolyps, it’s almost certainly ulcerative colitis. If they see patchy inflammation, cobblestone-like ulcers, and deep cracks in the lining? That’s Crohn’s. Biopsies help too. In UC, inflammation is only in the top layers. In Crohn’s, you’ll see granulomas-tiny clusters of immune cells-that show up in about 30% of cases. They’re rare in UC. Blood and stool tests add clues. A stool test for calprotectin (a marker of gut inflammation) is high in both, but more consistently so in UC. A blood test for pANCA antibodies is positive in 60-70% of UC patients, but only 10-15% of Crohn’s patients. That’s a strong hint. For unclear cases, doctors use MRI or capsule endoscopy. If the small intestine is inflamed and the colon looks fine? That’s Crohn’s. If the colon is the only problem? That’s UC.What Treatments Work Best
Both conditions use similar drugs-5-ASAs, steroids, immunomodulators, biologics-but how they’re used differs. For mild-to-moderate ulcerative colitis, enemas and suppositories with 5-ASA drugs (like mesalamine) work wonders. Since the problem is only in the colon, you can deliver the medicine right where it’s needed. About 60-80% of people go into remission with this approach. Crohn’s disease? You need drugs that work systemically. Oral or injected meds that travel through your whole body. Azathioprine or methotrexate help about half of patients within a few months. Biologics like infliximab or adalimumab work better for Crohn’s than for UC. In trials, about 35% of Crohn’s patients hit remission with these drugs after a year, compared to 25% for UC. Surgery is a last resort for both-but the outcome is worlds apart. For UC, removing the colon is a cure. For Crohn’s, it’s a temporary fix.What Patients Actually Experience
Real people with these conditions report different daily struggles. People with ulcerative colitis often say they live in fear of sudden, urgent bowel movements. About 87% report urgency. Rectal bleeding? That’s the norm for 75% of them. People with Crohn’s? They worry more about nutrition. Since their small intestine is often affected, they struggle to absorb vitamins, minerals, and calories. Weight loss and fatigue are common. Many need supplements or even tube feeding. Triggers vary too. On patient forums, UC patients point to stress as their biggest flare trigger. Crohn’s patients? They blame specific foods-dairy, high-fiber veggies, spicy meals. That’s not because food causes the disease, but because inflamed guts react badly to certain textures and fats.
Solomon Ahonsi
February 3, 2026 AT 07:11This article reads like a textbook someone forced to summarize at 3 a.m. while high on coffee. I’ve had Crohn’s for 12 years and no one ever explained it like this - but honestly? Most docs don’t even know the difference themselves. Just give me the pill and shut up.
Also, why does every medical article feel like it’s trying to win a Pulitzer? Just tell me what to avoid eating and when to call 911.
Also also - FMT? Poop transplants? I’m not paying $10k for someone else’s diarrhea to fix mine. No thanks.
George Firican
February 4, 2026 AT 01:47The distinction between Crohn’s and ulcerative colitis isn’t merely anatomical - it’s existential. One is a rebellion confined to the colon, a localized uprising against the body’s own lining; the other is a nomadic insurgency, wandering through the digestive tract like a disaffected spirit seeking its next battleground. The mucosa is not just tissue - it’s the boundary between self and invasion. When Crohn’s punches through all layers, it doesn’t just inflame - it redefines the architecture of survival. And yet, we treat both with the same blunt instruments: immunosuppressants, biologics, surgical amputations of hope. We don’t ask why the immune system turns traitor. We only ask how to silence it. But silence isn’t cure. It’s ceasefire. And ceasefires always end.
Perhaps the real question isn’t whether it’s Crohn’s or UC - but why our bodies, in their infinite, bewildering wisdom, chose this particular form of civil war to wage against us.