How to Talk to Your Doctor About Staying on a Brand Medication When Generics Are Available
 Dec, 7 2025
Dec, 7 2025
Switching from a brand-name medication to a generic can save money - but for some people, it can also mean worse symptoms, more side effects, or even dangerous health risks. If you’ve noticed something off after your pharmacy switched your prescription, you’re not imagining it. And you don’t have to accept it without a fight.
Why Some People Can’t Switch to Generics
Not all medications are created equal, even when they’re labeled as "bioequivalent." The FDA says generics must contain the same active ingredient and work the same way in the body. But here’s what they don’t always say: generics can have different fillers, dyes, or preservatives. For most people, that’s fine. For others, it’s a problem. Take levothyroxine, the drug used for hypothyroidism. Even tiny changes in how it’s absorbed can throw off your thyroid levels. A 2021 study found that switching from brand to generic levothyroxine led to abnormal TSH levels in nearly 1 in 5 patients. Same active ingredient. Different results. The same goes for warfarin, a blood thinner. One study showed a 17% spike in emergency room visits after patients switched between different generic versions. Why? Because the body’s response to small changes in absorption can be unpredictable - and life-threatening. Epilepsy patients report similar issues. On patient forums, stories like this are common: "I hadn’t had a seizure in five years on the brand. Three months after switching to generic Keppra, I had three in a row." That’s not coincidence. Studies confirm a 23% higher risk of seizure recurrence after switching to generics for certain anti-seizure drugs. If you’ve had a bad reaction - whether it’s a rash, stomach upset, dizziness, or a flare-up of your condition - write it down. Include dates, symptoms, and any lab results. That’s your evidence.What to Say to Your Doctor
Talking to your doctor about staying on brand isn’t about being difficult. It’s about being informed. Most doctors want what’s best for you - but they’re under pressure to prescribe generics. Your job is to give them the facts they need to advocate for you. Start with this: "I’ve had a bad experience with the generic version. Here’s what happened." Then, be specific:- "I switched to the generic version of my blood pressure pill in March. Within two weeks, my readings went from 120/80 to 150/95. When I went back to the brand, they dropped right back down."
- "I got a bad rash after taking the generic version of my antidepressant. The brand never caused that."
- "My blood levels for warfarin kept fluctuating after the switch. My INR jumped from 2.4 to 4.1 - that’s dangerously high. I’m worried about bleeding."
- Situation: "I’m here because I had a bad reaction to the generic version of my medication."
- Background: "I’ve been on the brand version for three years with no issues."
- Assessment: "I believe the generic is causing my symptoms to return."
- Recommendation: "Can we keep me on the brand name? I have records of my lab results and symptoms."
Insurance Is the Real Hurdle
Even if your doctor agrees you should stay on brand, your insurance might not cover it. That’s where things get tricky. Most health plans in New Zealand and the U.S. require you to try the cheaper generic first. If you want the brand, you need a prior authorization - and that means paperwork. Your doctor has to fill out forms explaining why the generic won’t work for you. Here’s how to make it easier:- Ask your doctor to write "Dispense as Written" or "DAW-1" on the prescription. That tells the pharmacy not to substitute.
- Provide your doctor with copies of your past pharmacy records showing when you switched and what happened.
- If you’ve had lab tests done, bring those results. Abnormal TSH, INR, or drug levels are powerful evidence.
What If Your Doctor Says No?
Sometimes, doctors say no because they’re overwhelmed or pressured by insurance. Don’t take it as the final answer. Ask: "Can we get a second opinion?" Or, "Can you refer me to a specialist who’s more familiar with this medication?" Some conditions - like epilepsy, thyroid disease, bipolar disorder, or organ transplants - require extra care. A neurologist, endocrinologist, or transplant specialist may be more willing to push back on insurance. You can also appeal directly to your insurance company. Most have a formal process. Write a letter. Attach your records. Mention that the FDA acknowledges differences in inactive ingredients can affect sensitive patients. Use the term "therapeutic inequivalence." It’s a real medical phrase. It carries weight.Know Your Rights
In New Zealand, pharmacists can substitute generics without asking - but you have the right to refuse. Tell the pharmacist: "I’m not switching. I need the brand." If they push back, say: "My doctor prescribed this brand for medical reasons. I’m not changing it without their approval." You’re not being difficult. You’re being responsible. Also, check if your medication is a specialty drug. Many newer treatments - especially for autoimmune diseases, cancer, or rare conditions - don’t have generics at all. If yours is one of them, you’re already on the brand. No need to worry.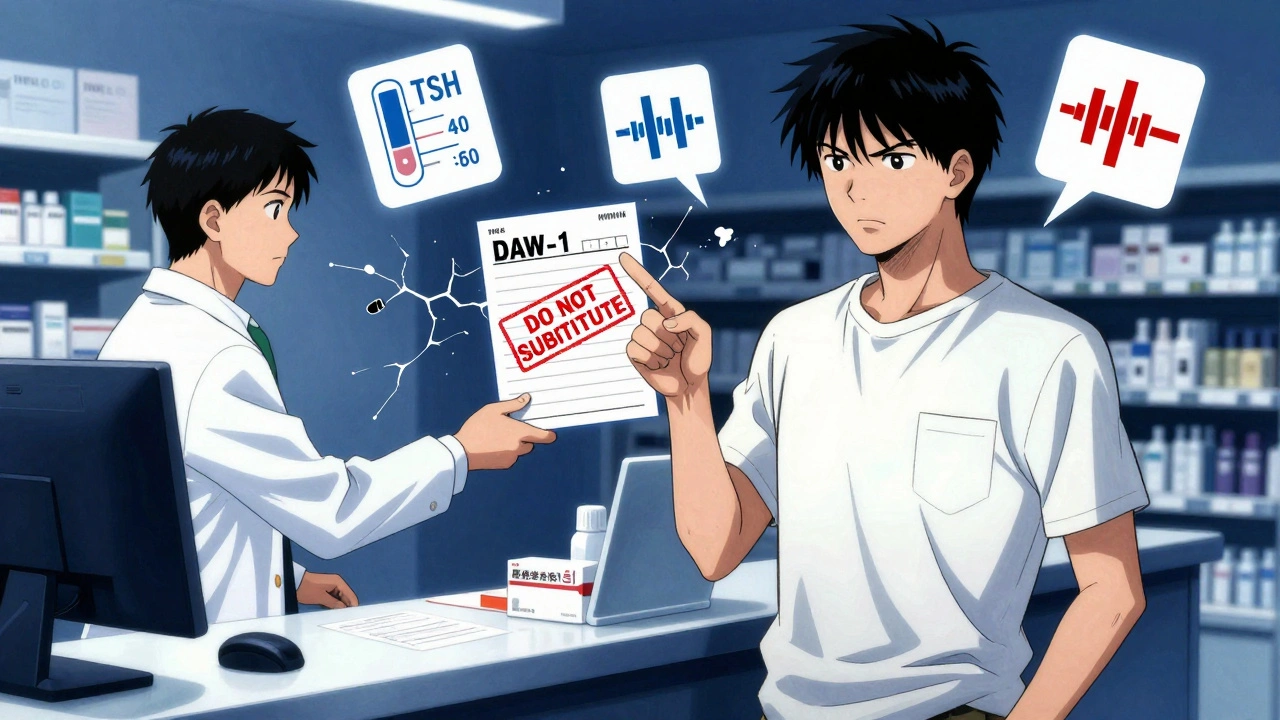
When Generics Are Fine
Let’s be clear: for most people, generics work perfectly. For blood pressure pills, cholesterol meds, antibiotics, and many others, switching saves money with no downside. The issue isn’t generics. It’s the blanket assumption that all drugs behave the same after a switch. That’s not true. And pretending it is puts patients at risk. If you’re on a medication with a narrow therapeutic index - meaning the difference between a safe dose and a harmful one is small - you need to be extra careful. These include:- Levothyroxine (for thyroid)
- Warfarin (blood thinner)
- Phenytoin, carbamazepine, valproate (for seizures)
- Lithium (for bipolar disorder)
- Cyclosporine (for transplants)
What to Do Next
If you’re thinking about staying on your brand medication, here’s your action plan:- Write down every time you switched to a generic and what happened - symptoms, dates, lab changes.
- Check your prescription. Does it say "Dispense as Written"? If not, ask your doctor to add it.
- Call your pharmacy. Ask them to confirm which version you’re getting - brand or generic. Keep a record.
- Bring your symptom log and lab results to your next appointment.
- Use the SBAR method to explain why you need the brand.
- If denied, appeal. Submit your documents. Be persistent.
Frequently Asked Questions
Can I ask my doctor to keep me on the brand medication even if a generic is available?
Yes, absolutely. You have the right to request the brand version if you’ve had problems with generics or if your condition requires precise dosing. Your doctor can write "Dispense as Written" on the prescription and submit documentation to your insurer to justify the need.
Why do some people have worse side effects on generics?
Generics must have the same active ingredient as the brand, but they can contain different inactive ingredients like dyes, fillers, or preservatives. Some people are sensitive to these - for example, lactose, gluten, or artificial colors. These can cause rashes, stomach upset, or even trigger flare-ups in conditions like epilepsy or thyroid disease.
Which medications are most likely to cause problems when switching to generics?
Medications with a narrow therapeutic index are the most sensitive. These include levothyroxine (for thyroid), warfarin (blood thinner), phenytoin and carbamazepine (for seizures), lithium (for bipolar disorder), and cyclosporine (for organ transplants). Even small changes in how your body absorbs these drugs can lead to serious health risks.
How can I prove to my insurance that I need the brand?
Collect evidence: lab results showing unstable levels (like TSH or INR), pharmacy records showing when you switched, a symptom diary with dates and severity, and any doctor’s notes. Submit this with your appeal. Insurance companies approve 72% of appeals when they have clear documentation.
Can my pharmacist switch my medication without telling me?
In many places, yes - unless your prescription says "Dispense as Written" or you’ve told them not to substitute. Always check the label when you pick up your prescription. If you see a different name than what your doctor prescribed, ask the pharmacist. You have the right to refuse a substitution.
What if my doctor won’t support me staying on the brand?
Ask for a referral to a specialist - like an endocrinologist, neurologist, or cardiologist - depending on your condition. Specialists often have more experience with these issues and are more likely to advocate for brand-name drugs when medically necessary. You can also request a second opinion.
Larry Lieberman
December 8, 2025 AT 15:08I literally cried reading this. My mom switched to generic levothyroxine and went from feeling fine to barely able to get out of bed. Her TSH went from 2.1 to 8.9 in 6 weeks. We had to fight the pharmacy AND the doctor. 🥲
Sabrina Thurn
December 9, 2025 AT 09:16As a clinical pharmacist, I’ve seen this too often. The FDA’s bioequivalence thresholds (80-125% AUC) are mathematically valid for population-level data but clinically meaningless for patients on narrow-therapeutic-index drugs. The inactive ingredients? Often the culprit. Lactose intolerance in a patient on levothyroxine? That’s not ‘patient noncompliance’ - that’s bad formulation design. We need labeling for excipient sensitivity, not just active ingredient equivalence.
Lisa Whitesel
December 10, 2025 AT 12:29People like you are why healthcare costs are out of control. If you can’t afford the generic, maybe you shouldn’t be on expensive meds at all. My cousin takes generic metformin and lives perfectly fine. Stop being dramatic.
Angela R. Cartes
December 11, 2025 AT 19:15OMG YES. I’ve been on brand Keppra for 8 years. Switched once because insurance forced it. Had a seizure in the shower. Called 911. Now I pay $200/month out of pocket because I refuse to gamble with my brain. 🙏 #BrandOrBust
iswarya bala
December 13, 2025 AT 16:38i had same issue with my epilepsy med... switched to generic n got dizzy all day... my doc didnt believe me till i showed him my log... now he fights for me too :) u r not alone
Raja Herbal
December 13, 2025 AT 21:47Oh so now it’s a conspiracy? The FDA is just lying to save Big Pharma money? I’ve been on generic warfarin for 12 years. My INR is stable. Maybe your doctor sucks, not the generic.
Andrea Beilstein
December 15, 2025 AT 14:04There’s a deeper question here - why do we treat human bodies like interchangeable parts in a machine? We accept that no two fingerprints are alike, yet we assume two pills with the same active ingredient will produce the same biological response. That’s not science. That’s industrial reductionism. The body isn’t a spreadsheet. It’s a symphony of chemistry, sensitivity, and memory. And when you change the tuning of one note - even slightly - the whole piece collapses. We’ve forgotten that medicine isn’t just about molecules. It’s about lived experience.
Ryan Brady
December 16, 2025 AT 05:12USA is the only country where people whine about paying $5 for a pill. In India, we’re happy to get any medicine at all. Get a job, stop being lazy, and take the generic. 🇺🇸😭
Courtney Black
December 18, 2025 AT 00:48It’s not about the drug. It’s about control. You don’t want to feel powerless. So you cling to the brand name like a security blanket. But the truth? The generic is just as good. You’re just scared. Scared that your body is unreliable. Scared that your illness is unpredictable. Scared that you’re not in charge. So you blame the pill. Not the system. Not your anxiety. Not the fact that medicine is still more art than science. You’re not special. You’re just afraid.