How to Recognize Depression’s Impact on Medication Adherence
 Dec, 29 2025
Dec, 29 2025
When someone is struggling with depression, taking pills every day can feel impossible-even when those pills are life-saving. It’s not laziness. It’s not forgetfulness alone. Depression rewires motivation, memory, and even how you experience side effects. If you’re a clinician, caregiver, or someone managing multiple medications, recognizing how depression quietly sabotages adherence isn’t just helpful-it’s critical.
Depression Doesn’t Just Make You Feel Low-It Breaks Your Routine
Think about your daily medication schedule: morning pills with breakfast, evening ones after dinner, maybe a midday dose. Now imagine waking up with no energy to get out of bed. Your thoughts are foggy. The idea of opening a pillbox feels overwhelming. That’s not non-compliance. That’s depression. Studies show depressed patients are 2.3 times more likely to miss doses of heart medications like ACE inhibitors, beta-blockers, and mineralocorticoid receptor antagonists. These aren’t vague trends-they’re statistically significant, adjusted for age, comorbidities, and education. Depression doesn’t just affect mood. It disrupts the cognitive functions needed to manage treatment: planning, remembering, prioritizing.How to Spot the Signs in Real Life
You don’t need fancy tools to notice when depression is interfering with medication use. Look for patterns:- Missed doses cluster around days with low energy or social withdrawal
- Patient says, “I feel worse since I started this,” even when clinical markers haven’t changed
- They stop refilling prescriptions without explanation
- Side effects like dry mouth, fatigue, or weight gain are described with disproportionate distress
The Numbers Don’t Lie: Adherence Rates in Depressed Patients
Data from the Cambridge University study using the Morisky Medication Adherence Scale (MMAS-8) tells a clear story:- Only 6% of depressed patients scored a perfect 8 (high adherence)
- 54% scored between 6 and 7.99 (moderate adherence-meaning they miss doses regularly)
- 39.8% scored below 6 (non-adherent-frequently skipping or stopping meds)
Why Side Effects Feel Worse When You’re Depressed
Depression doesn’t just make you forget pills-it makes you hyper-aware of every physical sensation. A 2014 study from the Canary Islands used the GARSI scale to measure how patients rated their side effects. Non-adherent patients scored significantly higher: 0.87 vs. 0.71 for those who stuck with their meds. This isn’t about the drugs being stronger. It’s about perception. Depression amplifies discomfort. A slight nausea becomes unbearable. A drowsy afternoon feels like a chemical prison. Patients aren’t irrational-they’re trapped in a feedback loop: side effects → feeling worse → believing the medication is harmful → stopping. Dr. Maria De las Cuevas put it plainly: “The subjective experience of side effects is amplified in depression.”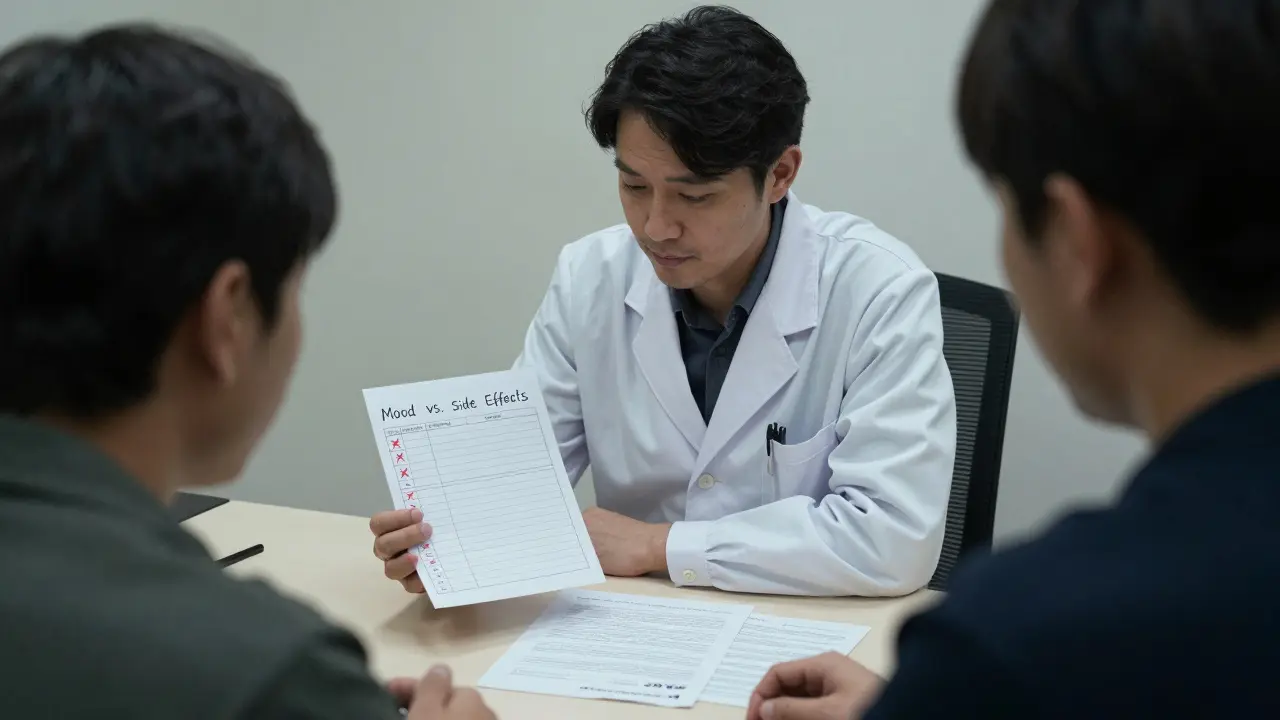
Screening Tools That Actually Work
You can’t guess who’s struggling. You need tools. Two are proven:- PHQ-9 - A 9-question depression screener. A score of 10 or higher means moderate depression-and a high risk of non-adherence.
- MMAS-8 - An 8-item questionnaire asking about missed doses, skipping pills, and stopping meds early. Scores below 6 mean non-adherence.
Early Warning Signs: The 20% Rule
The STAR*D trial gave us a practical red flag: if a patient misses more than 20% of their doses in the first two weeks of treatment, they’re 4.7 times more likely to have treatment failure. That’s not a suggestion-it’s a trigger. Don’t wait for a full relapse. Don’t assume they’ll “get used to it.” If doses are skipped early, probe gently: “I noticed you haven’t taken your pill for a few days. What’s been going on?” This isn’t about catching someone in a lie. It’s about catching a spiral before it pulls them under.Side Effect Mapping: A Simple Fix
Dr. George Alexopoulos at Weill Cornell Medicine recommends a low-tech solution: daily side effect mapping. Ask patients to keep a two-column log:- Left column: Mood (1-10)
- Right column: Side effects (e.g., drowsy, dry mouth, nausea)
Collaborative Care Works
The MAPDep study in Spain showed something powerful: when patients and doctors reviewed adherence together every two weeks, adherence jumped by 28.5% over a year. Not because they got new pills. Because they were heard. Depression thrives in silence. Adherence collapses without connection. Regular check-ins-whether in person, by phone, or via secure messaging-make patients feel seen. And when they feel seen, they’re more likely to stick with treatment.What’s Next: Digital Tools and Brain Science
New tools are emerging. Smartphone apps that track mood and pill intake have shown 82% accuracy in predicting a missed dose 72 hours ahead. That’s not sci-fi-it’s real, tested in 2024. Even more fascinating? Brain imaging. Dr. Helen Mayberg’s team found that depressed patients with low adherence show reduced activity in the dorsolateral prefrontal cortex-the part of the brain that handles planning and self-control. This isn’t just psychological. It’s neurological. Depression physically weakens the ability to follow through. The WHO is investing $15 million to build global protocols for recognizing this link by 2025. We’re moving beyond “just take your pills” to understanding the brain behind the behavior.What You Can Do Today
You don’t need to wait for new tech or big policy changes. Start here:- Ask every patient with a chronic condition: “How’s your mood been since you started this medication?”
- Use PHQ-2 at every visit. If they answer yes to one question, follow up with PHQ-9.
- Give them MMAS-8-just eight simple questions. It takes 2 minutes.
- When side effects are reported, don’t dismiss them. Ask: “How much does this affect your day?”
- Offer a simple log sheet. Two columns. Mood and side effects. No tech needed.
srishti Jain
December 29, 2025 AT 18:00Kelly Gerrard
December 31, 2025 AT 08:27Henry Ward
January 2, 2026 AT 00:32Joseph Corry
January 2, 2026 AT 11:41Colin L
January 2, 2026 AT 18:45Hayley Ash
January 3, 2026 AT 16:12kelly tracy
January 5, 2026 AT 08:52Cheyenne Sims
January 6, 2026 AT 13:59Shae Chapman
January 8, 2026 AT 10:34Nadia Spira
January 9, 2026 AT 23:28henry mateo
January 10, 2026 AT 11:34Kunal Karakoti
January 10, 2026 AT 16:15Glendon Cone
January 11, 2026 AT 12:03Aayush Khandelwal
January 12, 2026 AT 00:35