How to Read Pharmacy Allergy Alerts and What They Really Mean
 Dec, 8 2025
Dec, 8 2025
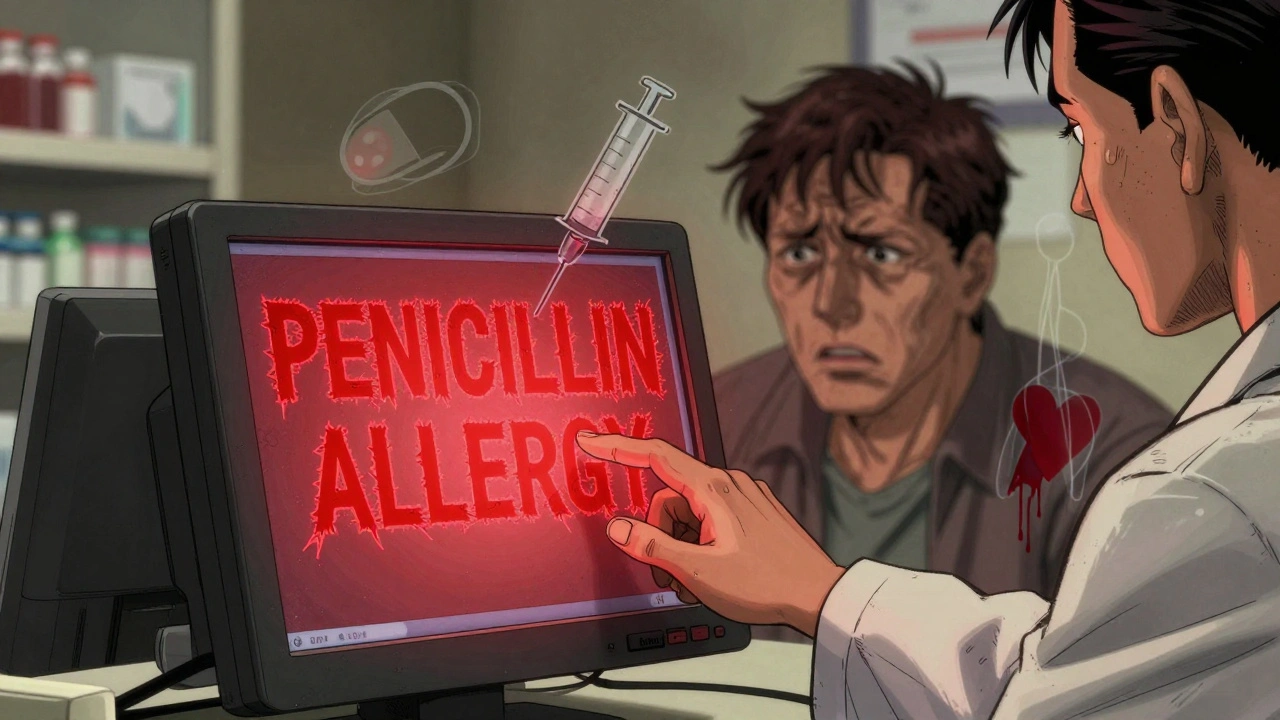
When you pick up a prescription, you might see a red or yellow pop-up on the pharmacist’s screen. It says: "Allergy Alert: Penicillin". Your heart skips a beat. Did you have a reaction? Is this safe? You’re not alone. These alerts happen thousands of times a day in pharmacies and hospitals, but most people - even many clinicians - don’t know how to read them properly.
Pharmacy allergy alerts aren’t just warnings. They’re automated guesses, often wrong, that can cause real harm - either by stopping you from getting a needed medicine, or by letting you take one you shouldn’t. Understanding them isn’t just helpful. It’s necessary.
What Exactly Is an Allergy Alert?
An allergy alert is a pop-up message generated by your pharmacy’s computer system when you’re prescribed or dispensed a medication that matches something in your documented allergy list. It’s not a diagnosis. It’s a flag.
These systems use databases like First DataBank to compare your listed allergies with the ingredients in new drugs. If you’ve ever written "penicillin allergy" on a form, that’s what triggers the alert. But here’s the catch: the system doesn’t know if your reaction was real, mild, or even an allergy at all. It just sees a match and sounds the alarm.
There are two main types of alerts:
- Definite allergy alerts: The drug contains the exact ingredient you listed (like amoxicillin matching your "penicillin allergy").
- Possible allergy alerts: The drug is in the same class as your listed allergy (like cefdinir being flagged because it’s a cephalosporin, and you have a "penicillin allergy").
Here’s the kicker: 90% of all alerts are possible allergy alerts - not direct matches. And most of them are unnecessary.
Why So Many Alerts Are Wrong
Most people who say they’re allergic to penicillin aren’t. Studies show that 90% of patients who report a penicillin allergy can actually take it safely. Many of those "allergies" were childhood rashes, stomach upset, or even just a bad reaction to an infection - not a true immune response.
But EHR systems don’t care. They see "penicillin allergy" and flag every beta-lactam antibiotic: amoxicillin, ampicillin, cephalexin, ceftriaxone - even if you’ve taken them before without issue. A 2023 study found that 63% of penicillin allergy alerts were triggered by reactions that were never confirmed as true allergies.
And it’s not just penicillin. NSAIDs like ibuprofen are flagged for "allergy" when the patient only had nausea or a headache. Antibiotics like vancomycin get flagged because someone once said "I’m allergic to antibiotics" - meaning they got sick once and assumed it was the drug.
The system doesn’t distinguish between:
- True allergic reaction: Immune system response - hives, swelling, trouble breathing, anaphylaxis.
- Adverse reaction: Side effect - nausea, dizziness, diarrhea, rash from sun exposure.
That’s why 95% of allergy alerts get overridden. Clinicians aren’t ignoring safety. They’re ignoring noise.
How to Read the Alert - Step by Step
When an alert pops up, don’t panic. Don’t just click "continue." Stop and ask:
- What’s the exact drug? Is it the one you were told you’re allergic to? Or just in the same family?
- What was your reaction? Was it hives? Swollen lips? Trouble breathing? Or was it just a stomach ache or rash that faded in a day?
- When did it happen? Did it happen within minutes or hours after taking the drug? Or was it days later? True allergies happen fast - usually under 1 hour.
- Was it ever tested? Have you ever had a skin test or oral challenge to confirm the allergy? Most people haven’t.
If your reaction was mild - like a rash that went away, or nausea - and it happened more than 10 years ago, the alert is likely outdated. If you’ve taken the same drug or a similar one since then without issue, the alert is almost certainly wrong.
Pharmacists and doctors are trained to ask these questions. But if you’re the patient, you can help. Say this: "I was told I’m allergic to penicillin, but I took amoxicillin last year and had no problem. Can we check if this is really a risk?"

The Real Danger: Alert Fatigue
When you see 10 alerts a day, and 9 of them are false, you stop paying attention. That’s called alert fatigue. And it’s deadly.
A 2020 study found that even life-threatening anaphylaxis alerts are overridden 75-82% of the time. Why? Because so many are false. A nurse in New Zealand told me about a patient who had a real anaphylactic reaction to penicillin in 2010. But the system kept flagging cefazolin - a cephalosporin - because of outdated cross-reactivity rules. The patient’s doctor kept overriding it, thinking it was another false alarm. Turns out, the patient had never had a true penicillin allergy. The real risk was never the cephalosporin. It was the delay in treating their infection with the right antibiotic.
Alert fatigue doesn’t just waste time. It kills.
What’s Being Done to Fix This?
Big changes are coming - slowly.
Starting in 2023, U.S. hospitals are required to document allergy reactions in detail - not just "penicillin allergy," but "hives and swelling 20 minutes after taking amoxicillin, treated with epinephrine." That’s a game-changer.
Systems like Epic and Cerner now use machine learning to predict which alerts are likely to be false. If a doctor overrides the same alert 20 times for the same patient, the system learns to stop showing it.
Some hospitals now offer free penicillin allergy testing. A simple skin test takes 20 minutes. If it’s negative, your allergy label is removed - and you’ll never get flagged again.
And here’s the best part: if you’ve been told you’re allergic to penicillin, you can ask your doctor for a referral to an allergist. Most people find out they’re not allergic at all.

What You Can Do Right Now
You don’t have to wait for the system to fix itself. Here’s what you can do today:
- Review your allergy list at every doctor visit. Ask: "Is this still accurate?"
- Be specific. Don’t say "I’m allergic to antibiotics." Say: "I got hives after taking amoxicillin in 2012. I’ve taken azithromycin since and had no issues."
- Ask about testing. If you’ve had a penicillin allergy label for years, ask if you can get tested. It’s safe, fast, and free in many places.
- Keep a personal list. Write down what drug, what reaction, when, and how severe. Bring it to every appointment.
One patient in Dunedin did this after years of being denied antibiotics. She wrote: "Penicillin - rash, 2008, no swelling or breathing issues. Took amoxicillin in 2021 - no reaction." Her doctor removed the alert. Next time she had a sinus infection, she got the right medicine - and got better in 3 days.
The Bottom Line
Allergy alerts aren’t bad. They’re just broken. They were built to catch the rare, life-threatening reaction. But they scream for every little blip.
The goal isn’t to ignore them. It’s to understand them. A true allergy is rare. A mislabeled side effect is common. And your life - and your health - depend on knowing the difference.
If you’ve been told you’re allergic to a drug, don’t assume it’s true. Ask. Check. Test. And never let a computer make your health decisions for you.
Are all allergy alerts accurate?
No. Up to 90% of pharmacy allergy alerts are triggered by cross-reactivity or mislabeled side effects, not true allergies. Most people who think they’re allergic to penicillin aren’t. Systems flag drugs based on broad categories, not individual reactions.
What’s the difference between an allergy and an adverse reaction?
An allergy involves your immune system - it can cause hives, swelling, trouble breathing, or anaphylaxis. An adverse reaction is a side effect - like nausea, dizziness, or diarrhea - that doesn’t involve your immune system. Only about 5-10% of drug reactions are true allergies.
Can I outgrow a drug allergy?
Yes. Many drug allergies, especially penicillin, fade over time. Studies show that 80% of people who had a penicillin allergy in childhood lose it within 10 years. The only way to know for sure is through testing.
Should I avoid all penicillin-like drugs if I’m allergic to one?
Not necessarily. The risk of cross-reactivity between penicillins and newer cephalosporins is less than 2%. Most systems still flag all of them, but current guidelines say it’s often safe to use later-generation cephalosporins even with a penicillin history - especially if your reaction was mild.
How can I get my allergy label removed?
Ask your doctor for a referral to an allergist. They can perform a skin test or oral challenge - both are safe and accurate. If the test is negative, your allergy label can be removed from your medical record, and you’ll never get flagged again.
Why do I still get alerts even after I told my doctor I’m not allergic?
Because your allergy list hasn’t been updated in the system. Always confirm your allergy list at every visit. Ask the pharmacist or nurse: "Is my allergy list up to date?" If it’s not, request a correction. Many systems don’t auto-update unless someone manually edits them.
Katherine Rodgers
December 10, 2025 AT 02:07so i got flagged for penicillin bc i had a rash at 7… turned out it was chickenpox. but now every doc thinks i’m allergic to everything. like bro, i took amoxicillin last year for a sinus infection and lived to tell the story. why does the computer hate me so much?
Evelyn Pastrana
December 11, 2025 AT 15:11my grandma had a penicillin alert for 40 years. she never even had a reaction. just said ‘i think it made me feel weird once.’ then she got tested-turns out she’s fine. now she takes antibiotics like candy and lives to annoy her doctors. if you think you’re allergic, get checked. it’s not a life sentence.
Arun Kumar Raut
December 13, 2025 AT 04:48in india, we don’t have these fancy alerts. we just tell the pharmacist what happened. if you got sick after a pill, they remember. no system needed. but i see why this happens in big hospitals. too many patients, too many drugs. still, if the machine can’t tell a rash from anaphylaxis, maybe it shouldn’t be making decisions.
Carina M
December 13, 2025 AT 23:48It is profoundly irresponsible to suggest that patients should self-diagnose or override clinically validated pharmacovigilance protocols. The integrity of the electronic health record is predicated upon standardized, evidence-based nomenclature. To encourage laypersons to dismiss alerts based on anecdotal recollection is not merely negligent-it is a dereliction of duty to public health.
Tejas Bubane
December 14, 2025 AT 01:1590% of alerts are wrong? wow. so the entire healthcare IT industry built a system that screams wolf 9 times out of 10 and expects people to listen. brilliant. now the real problem is that doctors are too lazy to update records. fix the data, not the alert volume. and stop pretending this is a safety feature. it’s a glorified spam filter with a stethoscope.
Ajit Kumar Singh
December 14, 2025 AT 04:09people dont know the difference between allergy and side effect and its their own fault. why do you think you know more than the system. i had a cousin die from anaphylaxis because someone said they werent allergic but they were. dont be stupid. trust the machine. if it says penicillin dont take it. period
Lisa Whitesel
December 15, 2025 AT 13:52Stop pretending you're a doctor. If you didn't get tested, you're not cleared. Your anecdote isn't data. The system is there for a reason. You're lucky you didn't die.
Larry Lieberman
December 17, 2025 AT 08:34sooooo… if i had a rash from amoxicillin in 2005 but took it again in 2020 and was fine… does that mean the system is just being dramatic? 😅 i feel like i’ve been ghosted by my own medical record. also can we make these alerts less red? they look like a fire alarm in a horror movie.
Olivia Portier
December 18, 2025 AT 11:10my sister got flagged for penicillin bc she threw up once after antibiotics-turns out she had food poisoning. she’s been asking her docs to fix it for 8 years. no one listens. so now she just brings her own handwritten list to every appointment. it’s ridiculous that we have to be our own record keepers. but hey, at least we’re not dead. yet.
Tiffany Sowby
December 18, 2025 AT 18:04why are we letting Americans think they know more than machines? in my country, doctors don’t ask questions-they just follow the alert. if you’re not allergic, why did you ever say you were? you’re the problem. stop being so casual about your health. this isn’t a TikTok trend.
Asset Finance Komrade
December 19, 2025 AT 21:09One might posit that the algorithmic architecture of modern pharmacovigilance systems reflects a deeper epistemological crisis in post-industrial medicine: the substitution of heuristic certainty for phenomenological nuance. The patient, once sovereign in their bodily narrative, is now reduced to a data point in a probabilistic schema. Is this liberation-or subjugation by the very tools meant to protect us?
Jennifer Blandford
December 21, 2025 AT 12:14i just got my penicillin allergy removed after a 20-minute skin test. zero pain. zero drama. now i can actually get treated for infections instead of being stuck with clindamycin that gives me diarrhea for a week. if you’ve had an allergy label for more than 5 years… go get tested. your future self will high-five you. 🙌