How to Discuss Expired Medication Use During Disasters or Shortages
 Feb, 9 2026
Feb, 9 2026
When a disaster hits-whether it’s a hurricane, wildfire, or power grid failure-people don’t just lose power or water. They lose access to their medicines. And when pharmacies are closed, delivery routes are blocked, or hospitals are overwhelmed, many are left with one question: Can I still use my expired pills? It’s not a theoretical concern. In the aftermath of Hurricane Maria, nearly half of Puerto Ricans relied on expired drugs. In California wildfires, over 60% of evacuees did the same. This isn’t about being reckless. It’s about survival. And knowing when, how, and why to use expired medication could save a life.
Expiration Dates Aren’t What You Think
Most people assume that if a pill’s expiration date passed yesterday, it’s now dangerous or useless. That’s not true. The FDA requires manufacturers to test drugs for stability under controlled conditions-typically 25°C and 60% humidity. The expiration date is the last day they guarantee full potency under those ideal conditions. It’s not a "use-by" date for safety. Many medications remain effective for years beyond that date.
Studies from the FDA’s Shelf Life Extension Program show that 88% of military stockpiled drugs retained potency well past expiration-some by over a decade. But here’s the catch: those were sealed, climate-controlled, military-grade storage conditions. Your medicine cabinet? Not the same. Heat, humidity, and moisture change everything.
Not All Expired Medications Are Equal
Some drugs degrade slowly. Others turn risky fast. The difference isn’t just academic-it’s life-or-death.
- Solid tablets like ibuprofen, acetaminophen, or aspirin often keep 90%+ potency for 1-5 years after expiration if stored dry and cool. A University of Utah study found acetaminophen still 95% effective at four years out.
- Liquid antibiotics like amoxicillin suspension lose potency quickly-up to 50% within six months of expiration. But if it’s the only option during a crisis, using it may still be better than nothing.
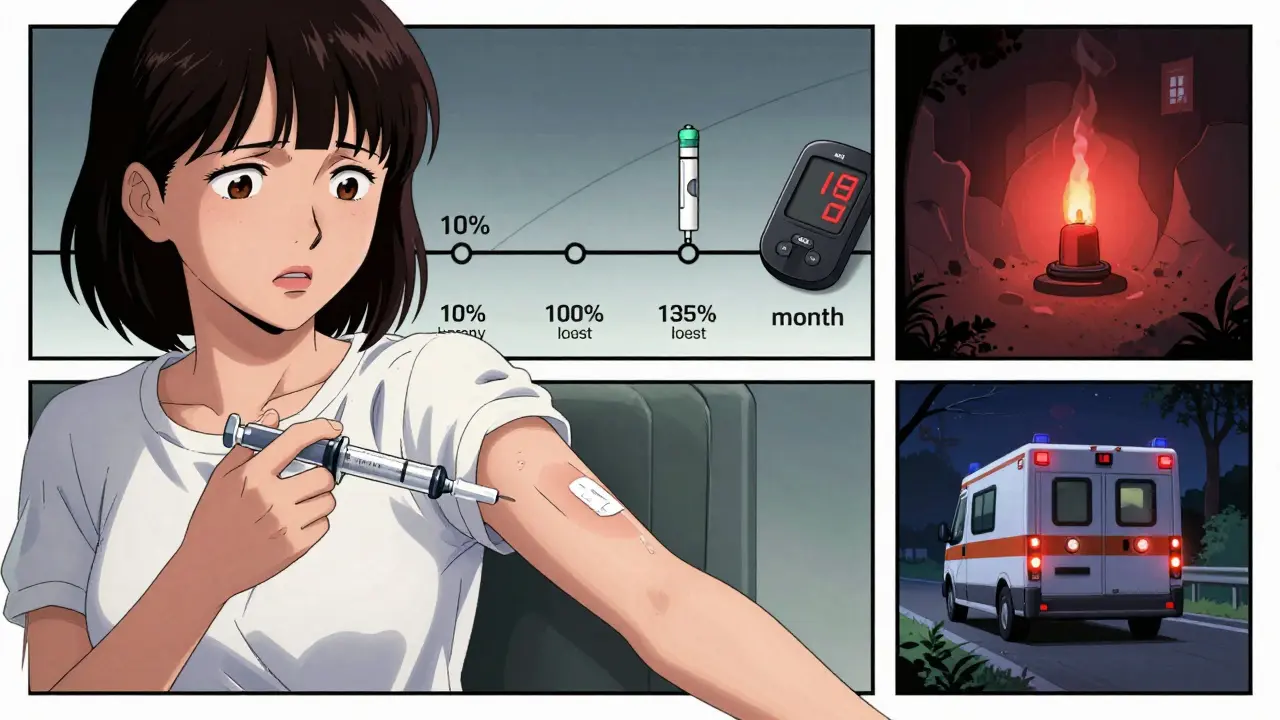
- Insulin degrades rapidly. At room temperature, it loses about 10% potency per month after expiration. For diabetics, this isn’t just a nuisance-it can mean dangerous blood sugar swings.
- Epinephrine auto-injectors (EpiPens) lose 2-4% potency per month. One verified pharmacist on Reddit reported seeing 60% effectiveness from a 6-month-expired EpiPen in anaphylaxis. Still, doubling the dose might be needed.
- Nitroglycerin tablets, used for heart attacks, lose half their strength within three months of opening. If you’re having chest pain and only have expired nitro, use it-but call for help immediately.
- Tetracycline is a hard no. Expired tetracycline can degrade into toxic compounds linked to kidney damage. There are 17 documented cases since 2000.
- Warfarin (blood thinner) becomes unpredictable after expiration. INR levels can spike unpredictably, increasing bleeding risk by 300%.
The National Academy of Medicine put it simply: for critical drugs like insulin or epinephrine, the risk-benefit ratio is 1:0.2-meaning five times more risk than benefit. For painkillers? 1:3.5. That’s a no-brainer.
Check the Physical Condition First
Before you even think about taking an expired pill, look at it. Smell it. Feel it.
The FDA says discard any medication that shows:
- Discoloration (yellow, brown, or cloudy)
- Cracking, crumbling, or sticking together
- Unusual odor (rancid, sour, chemical)
- Changed texture (liquid that’s thickened, tablets that are powdery)
And if it was exposed to floodwater? Pitch it. A 2022 FDA study found 92% of medications submerged for 24 hours had bacterial contamination. Same goes for anything left in a hot car for two days. Heat above 86°F (30°C) accelerates chemical breakdown by 15-25%.
When Is It Okay to Use Expired Medication?
There’s no universal rule. But experts agree on this: use expired meds only when there’s no alternative and the consequences of not using it are worse.
Here’s a practical decision tree:
- Is this life-saving? (Epinephrine, insulin, heart meds, seizure drugs) → Use only if absolutely necessary, and with extreme caution.
- Is this symptom-relieving? (Painkillers, antihistamines, antacids) → Usually safe for up to 1-5 years past expiration if stored well.
- Is this for infection? (Antibiotics) → Use within 1 year if solid form, stored dry. Avoid if liquid or if you’re immunocompromised.
- Is this for chronic disease? (Blood pressure, diabetes, thyroid) → Avoid unless no other option. The risk of under- or over-treatment is too high.
- Is there a telehealth option? → Even if you’re in a remote area, try to connect with a pharmacist or doctor via phone or text. Many states allow pharmacists to issue emergency 72-hour supplies without a prescription.
During Hurricane Ida, 47 cases were documented where expired albuterol inhalers gave 50-70% relief for asthma attacks-within a year of expiration. But in Texas, 12 cases of insulin treatment failure during power outages led to hospitalizations. Context matters.
What Experts Really Say
Dr. Sandra Kweder, Deputy Director of the FDA’s Center for Drug Evaluation and Research, said in a 2023 webinar: "In life-threatening situations with no alternatives, using certain expired medications may be preferable to receiving no treatment at all-but this should be a last-resort decision made with medical guidance when possible."
The American Medical Association’s 2022 guidelines allow antibiotics for life-threatening infections to be used up to one year past expiration-with adjusted dosing. But the American College of Emergency Physicians warns against expired bronchodilators for asthma attacks beyond six months. Why? Failure rates jump. You don’t want to be the person who used an expired inhaler and still couldn’t breathe.
NIH research in Clinical Infectious Diseases found expired ciprofloxacin still worked against E. coli at two years-but only 42% as effective against Pseudomonas. That’s why knowing the infection matters. Not all bugs are the same.
Real Stories from Real Disasters
After the 2020 California wildfires, a UC San Francisco survey of 312 evacuees found:
- 63% used expired meds
- 89% said pain relief from ibuprofen (up to 2 years expired) worked fine
- 37% had inadequate blood pressure control with expired lisinopril
One man, 68, used his 18-month-expired blood pressure pill for three days. His systolic pressure jumped from 120 to 160. He didn’t know until he got to a temporary clinic.
On Reddit’s r/Preppers, a verified pharmacist wrote: "I’ve seen patients use 6-month expired epinephrine with 60% effectiveness. Better than nothing. Double the dose if you can." That’s not advice you’ll find on a drug label. But it’s real-world experience from the front lines.
Meanwhile, a Johns Hopkins study found 28% of disaster survivors using expired antibiotics developed resistant infections-compared to 8% with fresh ones. Expired doesn’t always mean weak. Sometimes, it means dangerous.
What You Can Do Now
Don’t wait for a disaster to figure this out.
- Store meds properly: Keep them in a cool, dry place-not the bathroom or a hot car. A closet shelf is better than a medicine cabinet.
- Rotate your stock: Every six months, check your pills. Use what’s expiring soon. Replace it. Keep a 30-day supply of critical meds on hand.
- Know your drugs: Make a list of what you take, why, and whether it’s critical (insulin, EpiPen, warfarin) or non-critical (ibuprofen, antihistamine).
- Know your options: In 48 states, pharmacists can legally dispense emergency supplies for 72 hours without a prescription during declared emergencies. Ask your pharmacist what they can do.
- Get trained: If you’re a caregiver, a first responder, or just someone who wants to be prepared, ask about emergency medication training. Only 61% of community pharmacists have completed required training. Don’t assume they know.
The Bigger Picture
There are 297 active drug shortages in the U.S. as of late 2023. Nearly half are for critical care meds. Disasters make this worse. Pharmacy closures average 37% in disaster zones. The system isn’t broken-it’s fragile.
The FDA, CDC, and NIH are working on solutions: new field-testing tools that can check drug potency in five minutes, better packaging to extend shelf life, and updated emergency protocols. But until those are everywhere, the responsibility falls on you.
You can’t control when the next disaster hits. But you can control how prepared you are. Keep your meds in good shape. Know what’s safe to use. Understand the risks. And if you ever have to use something expired-use it wisely.
Sonja Stoces
February 9, 2026 AT 18:01Annie Joyce
February 11, 2026 AT 03:57