Herpes Simplex on Skin: How to Prevent Recurrences and Care for Outbreaks
 Dec, 6 2025
Dec, 6 2025
Herpes simplex on the skin isn’t just a nuisance-it’s a lifelong condition that affects millions. Whether it’s a cold sore on your lip or a genital outbreak, the virus doesn’t go away after the first flare-up. It hides in your nerves and comes back when you least expect it. The good news? You can significantly reduce how often outbreaks happen and make them much less severe. This isn’t about magic fixes or home remedies that don’t work. It’s about science-backed strategies that actually help people live better with herpes simplex.
What Causes Herpes Simplex Recurrences?
Herpes simplex virus (HSV) comes in two types: HSV-1 usually causes cold sores around the mouth, and HSV-2 is more common in genital areas. But both can show up anywhere. After your first infection, the virus moves into nerve cells and stays there forever. It’s not active all the time. It waits. Then something triggers it to wake up and travel back to the skin.
Common triggers include:
- Stress-emotional or physical
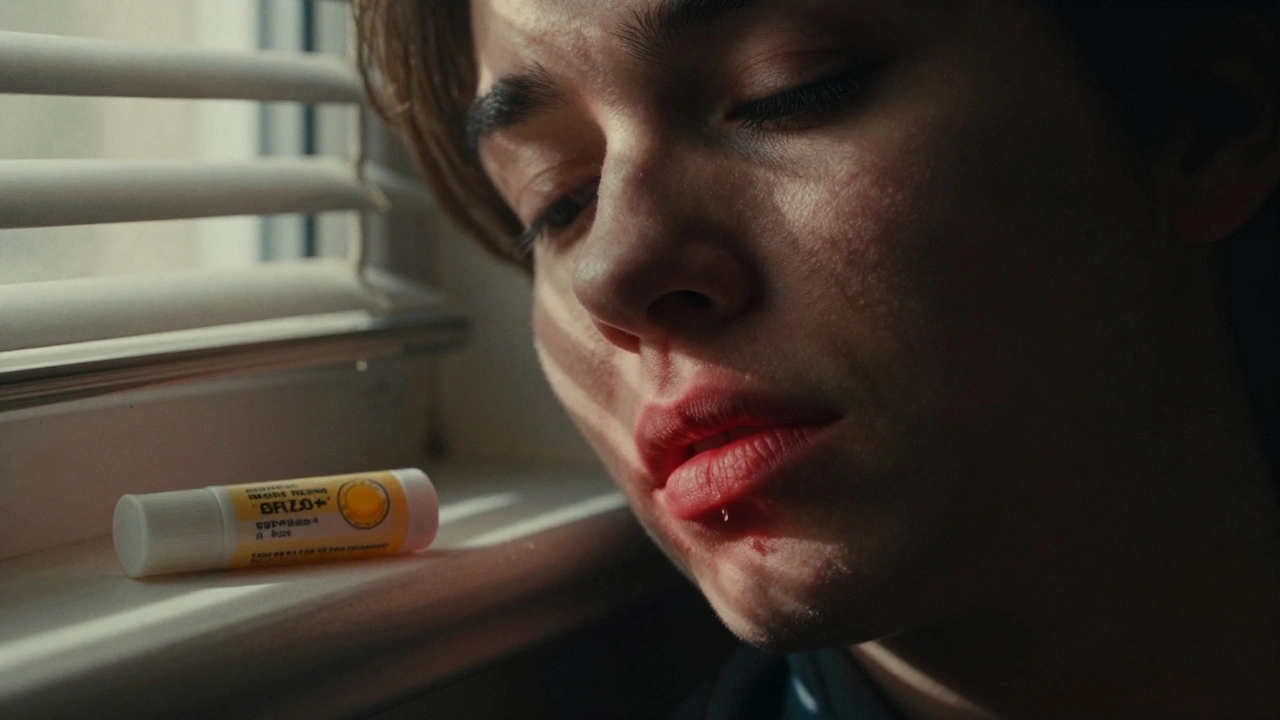
- UV exposure from sunlight or tanning beds
- Illness or fever
- Hormonal changes (like menstruation)
- Physical trauma (like dental work or laser skin treatments)
- Fatigue or poor sleep
One study found that 68% of people with HSV report stress as their top trigger. Another found that 76% of users reduced outbreaks by using SPF 30+ lip balm daily. That’s not coincidence-it’s protection.
Antiviral Medications: The Gold Standard for Prevention
There are three main antiviral drugs used to manage herpes simplex: acyclovir, valacyclovir, and famciclovir. These aren’t cures, but they’re the most effective tools we have to stop outbreaks before they start.
Valacyclovir (Valtrex) is often preferred because it’s absorbed better by the body than acyclovir. You take less of it, less often. For people who get six or more outbreaks a year, daily suppressive therapy with valacyclovir 500mg once a day reduces recurrences by 70-80%. That’s not a small improvement-it’s life-changing.
For cold sores, the CDC recommends:
- Acyclovir 400mg twice daily for prevention after sun exposure
- Valacyclovir 500mg twice daily for similar results, with fewer pills to take
For genital HSV-1 (which is less likely to recur than HSV-2), suppressive therapy isn’t always recommended unless outbreaks are frequent. Why? Because HSV-1 genital outbreaks happen only about 0.2 times per year on average-much less than HSV-2’s 4-5 times. So for many, it’s not cost-effective.
Cost matters. In the U.S., valacyclovir can run $370 a month without insurance. That’s why some people skip doses. But here’s the catch: skipping doses increases your risk of outbreaks-and transmission.
Episodic Therapy: Catching Outbreaks Early
If you don’t take daily meds, there’s still a powerful option: episodic therapy. This means taking antivirals only when you feel an outbreak coming on.
The key word is early.
Most people feel a warning sign before the blister appears-a tingling, burning, or itching sensation. That’s your signal. Start your medication right then. The CDC says taking valacyclovir 2g twice in one day (12 hours apart) at the first sign of prodrome cuts healing time from 5.2 days to 4.3 days. Start after the sore appears? You lose about half the benefit.
For dental work, laser treatments, or other skin procedures, taking valacyclovir 2g one hour before the appointment reduces outbreak risk from 20.6% to 11.3%. That’s a 46% drop. Dermatologists now screen patients for herpes history before any invasive procedure. If you’ve had cold sores before, you’re at risk-even if it’s been years.
What Doesn’t Work (And Why)
There’s a lot of misinformation out there. Topical creams like acyclovir 5% ointment? They don’t prevent outbreaks. They might slightly shorten healing time if applied early, but they don’t stop the virus from reactivating.
Essential oils, lysine supplements, or “natural” remedies? No solid evidence they prevent recurrences. Some people swear by them, but studies show no consistent benefit. Lysine, for example, was once popular-but large reviews found no significant effect on outbreak frequency.
And don’t rely on episodic therapy if you only have 1-2 outbreaks a year. It’s not worth the cost or hassle. Daily suppressive therapy only makes sense if you’re having six or more outbreaks annually.
Trigger Management: Real-World Strategies
Medication helps, but managing triggers is where you take control.
- Sun protection: Use SPF 30+ lip balm every day, even in winter. UV rays are a top trigger for oral herpes.
- Stress reduction: Practice mindfulness, exercise regularly, or talk to a counselor. One Reddit community found that stress caused outbreaks within 48 hours for most users.
- Sleep and immunity: Don’t burn out. Poor sleep weakens your immune system and makes outbreaks more likely.
- Hygiene: Don’t touch active sores. Wash your hands immediately if you do. Avoid sharing towels, razors, or lip balm.
- Medical procedures: Always tell your dentist, dermatologist, or aesthetic provider if you’ve ever had herpes. They can prescribe pre-treatment antivirals.
Zinc supplements (15-30mg daily) helped 63% of people in one survey reduce outbreak severity. Not a cure, but a helpful tool. Talk to your doctor before starting any supplement.
Transmission Risk: You Can Still Spread It
Even if you’re on daily antivirals, you can still pass the virus to others. Studies show that despite suppressive therapy, about 4-5% of serodiscordant couples (one partner has HSV, the other doesn’t) still see transmission.
That’s why it’s not just about you-it’s about others too. Avoid kissing or sexual contact during outbreaks. Even without visible sores, the virus can shed (come out of nerves) without symptoms. Daily antivirals reduce shedding by 70-90%, but not completely.
Use condoms and dental dams during sex. Talk openly with partners. There’s no shame in saying, “I have herpes. I manage it with medication, but I want to be safe.”
Long-Term Outlook and New Developments
Herpes simplex isn’t going away. It’s estimated that 67% of people under 50 have HSV-1 globally. But the tools we have now are better than ever.
There’s no approved vaccine yet. Two candidates (GEN-003 and HSV529) showed promise in trials but didn’t meet their main goals in 2023. Research continues.
New drugs like pritelivir are approved for rare cases of drug-resistant HSV, but only for people with weakened immune systems.
Looking ahead, long-acting injectable antivirals that last 90 days are in phase II trials. That could change everything-no more daily pills. But it’s still years away.
For now, the best approach is simple: know your triggers, use antivirals wisely, and protect yourself and others.
When to See a Doctor
See a healthcare provider if:
- You’re having more than six outbreaks a year
- Outbreaks are lasting longer than two weeks
- You have sores near your eyes (can cause vision damage)
- You’re pregnant or planning to be
- Your immune system is weakened (from HIV, chemo, etc.)
Most people can manage herpes simplex with their primary care provider. You don’t need a specialist unless complications arise.
Can herpes simplex be cured?
No, herpes simplex virus cannot be cured. Once you’re infected, the virus stays in your nerve cells for life. But it doesn’t always cause symptoms. With proper care, most people experience fewer, milder outbreaks-or none at all. The goal isn’t to eliminate the virus, but to control it.
Is it safe to take antivirals long-term?
Yes, for most people. Acyclovir, valacyclovir, and famciclovir are safe for years of use. The biggest risk is kidney issues in people with pre-existing kidney disease or those taking high doses. Your doctor can check your kidney function with a simple blood test. For healthy individuals, long-term use is considered very safe.
Do I need to tell my partner I have herpes?
Yes. Ethically and practically, you should. Even with medication, there’s still a small chance of transmission. Being open helps your partner make informed choices about protection. Many people find that honesty strengthens relationships. Support groups and counselors can help you have this conversation if you’re nervous.
Can I get herpes from sharing a towel or toilet seat?
It’s extremely unlikely. Herpes simplex spreads through direct skin-to-skin contact with an active sore or during viral shedding. The virus doesn’t survive long on surfaces like towels, toilet seats, or doorknobs. You’re far more at risk from kissing, oral sex, or skin contact during an outbreak than from indirect contact.
Why do I keep getting outbreaks even when I take meds?
No treatment works 100%. Even with daily antivirals, stress, sun exposure, illness, or hormonal changes can still trigger outbreaks. If you’re still having frequent outbreaks despite medication, talk to your doctor. You might need a higher dose, a different drug, or help identifying hidden triggers. Sometimes, it’s not the meds-it’s the lifestyle.
Is herpes simplex the same as shingles?
No. Herpes simplex (HSV) and shingles (caused by varicella-zoster virus) are completely different viruses. HSV causes cold sores and genital sores. Shingles causes a painful, blistering rash along a nerve pathway, usually on one side of the body. They’re not related, and having one doesn’t mean you’ll get the other.
Next Steps for Managing Herpes Simplex
Start today:
- Track your outbreaks for 3 months. Note when they happen and what you were doing before.
- Use SPF 30+ lip balm daily-even on cloudy days.
- Learn your prodrome signs. That tingling? That’s your cue.
- If you have six or more outbreaks a year, ask your doctor about daily suppressive therapy.
- Talk to your dentist or dermatologist before any procedure that breaks the skin.
- Reach out to a support group. You’re not alone.
Herpes simplex doesn’t define you. With the right approach, you can live a full, healthy life-with fewer outbreaks and more confidence.
brenda olvera
December 7, 2025 AT 20:29Just started using SPF 30 lip balm daily after reading this and holy crap my cold sores have vanished. No more hiding in summer. This is the first thing that actually worked for me after 12 years of trying everything from lysine to tea tree oil. Seriously just buy the damn balm.
Chris Park
December 8, 2025 AT 00:41Let me guess-big pharma paid you to write this. Valacyclovir? That’s just a money grab. The virus is a bio-weapon designed to control populations. Look at the stats: 67% of people under 50 have HSV-1. Coincidence? Or is this a slow-release population control program disguised as a medical condition? They don’t want you healthy-they want you dependent.
Myles White
December 8, 2025 AT 16:19I’ve been on daily valacyclovir for three years now and honestly it’s been a game-changer. I used to get six to eight outbreaks a year-mostly after stress or sun exposure. Now I get maybe one every 18 months, and even that’s mild. The cost is brutal without insurance, but I’ve found generic versions through Canadian pharmacies that cut the price by 70%. Also, the idea that HSV-1 genital outbreaks are rare is spot on-I had one once, never again. It’s not the monster people make it out to be. You just need to treat it like a chronic condition, not a moral failure.
Inna Borovik
December 10, 2025 AT 07:06There’s a massive flaw in the claim that SPF 30+ lip balm reduces outbreaks by 76%. That study was a 12-person observational survey with no control group. Also, the CDC doesn’t actually recommend acyclovir 400mg twice daily for sun-triggered outbreaks-that’s an off-label suggestion from a 2015 dermatology blog. This article is dangerously oversimplified. If you’re going to cite stats, cite the actual peer-reviewed papers, not Reddit threads and press releases.
joanne humphreys
December 10, 2025 AT 23:54I had my first outbreak after a breakup and thought I was dying. Then I learned it’s just a virus that’s been around since ancient Rome. I stopped seeing it as a punishment and started seeing it as a signal-my body’s telling me to slow down. I started meditating, sleeping better, and using sunscreen religiously. Outbreaks dropped from monthly to maybe once a year. It’s not about perfection. It’s about listening to your body. You’re not broken. You’re human.
Jackie Petersen
December 11, 2025 AT 04:51Why are we even talking about this like it’s normal? Everyone knows herpes is a dirty disease. You should’ve been more careful. Why are we giving out medical advice like it’s a yoga class? Just don’t sleep around and you won’t get it.
Nigel ntini
December 12, 2025 AT 11:49Brooke Evers nailed it. This isn’t about shame-it’s about awareness. I used to avoid dating because I was terrified of telling people. Then I started saying, ‘I have herpes, I take meds, and I use protection.’ Guess what? Most people were like, ‘Oh cool, same as me.’ Seriously, open up. You’d be shocked how many people have it and just don’t talk about it. The stigma kills more than the virus.
Saketh Sai Rachapudi
December 12, 2025 AT 11:55U guys r so dumb. Herpes is just a test from god to see if u r pure. Lysine works better than pills. I took 3000mg daily and never had a sore in 5 years. Also sunblock is for weak people. God protects the faithful. And why are u listening to america? India has been curing this with turmeric for 5000 years. Stop trusting big pharma.
Dan Cole
December 14, 2025 AT 01:33Let’s be brutally honest: herpes simplex isn’t a medical condition-it’s a social construct engineered to normalize lifelong vulnerability. We’ve been conditioned to believe that suppression equals control, but what if the real rebellion is accepting the virus as part of our biological identity? The antivirals are a Band-Aid on a bullet wound. The real question isn’t ‘how do I prevent outbreaks?’-it’s ‘how do I stop fearing myself?’ The virus doesn’t define you, but your panic about it? That’s the real prison.
Brooke Evers
December 14, 2025 AT 15:13For anyone feeling alone with this: you’re not. I’ve been on suppressive therapy for 7 years. I’ve had one outbreak since. I’ve dated, kissed, had sex, traveled, laughed, cried. I’m not ‘damaged.’ I’m just someone who takes a pill every day like millions take blood pressure meds. Don’t let fear silence you. Talk to your doctor. Get tested. Use sunscreen. Tell your partner. And if you’re scared to say it out loud-write it down first. I did. It got easier. You’ve got this.