Heartburn & Tummy Ache: Why They’re Linked and How to Find Relief
 Sep, 30 2025
Sep, 30 2025
Heartburn & Tummy Ache Symptom Checker
Check the symptoms you're experiencing to see if they might be linked and what could be causing them.
Symptoms You Have:
Common Triggers:
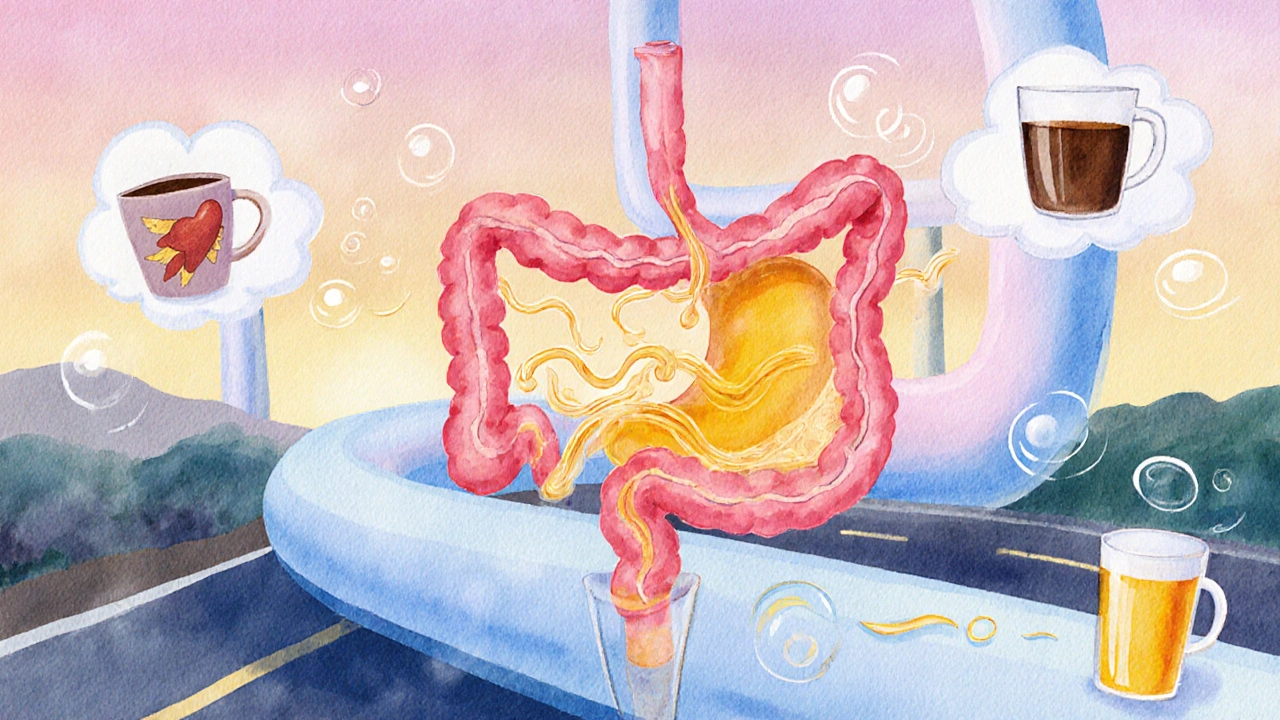
Ever felt a burning sensation behind your breastbone and, minutes later, a cramp in your belly? You’re not imagining it-those two symptoms often walk hand‑in‑hand. Below you’ll learn why Heartburn is a burning feeling caused by stomach acid that backs up into the esophagus and a tummy ache (also called abdominal pain) is any discomfort in the abdominal area, ranging from mild gurgle to sharp stabbing pain often share the same culprits, and what practical steps you can take for quick heartburn relief and a calmer gut.
What’s really happening inside?
To see the connection, picture the digestive tube as a highway. Food travels from the Stomach a muscular organ that churns food and mixes it with gastric acids up into the Esophagus the tube that carries swallowed food from the throat to the stomach. At the junction sits the Lower Esophageal Sphincter (LES) a ring of muscle that normally stays closed to keep stomach acid where it belongs. When the LES relaxes at the wrong time, acidic juice spills back-this is the classic acid reflux the backward flow of stomach acid into the esophagus that triggers heartburn.
But the LES isn’t a one‑way gate. It also influences pressure in the upper stomach. When it’s weak, not only does acid climb, but gas and partially digested food can sit longer, leading to bloating and the cramping we label as a tummy ache. In many cases the same trigger-whether it’s a big meal, spicy chili, or a stressful day-hits both the LES and the stomach’s ability to empty properly.
Common culprits that spark both symptoms
Here’s a quick checklist of the usual suspects:
- Overeating: Large meals stretch the stomach, increasing pressure on the LES.
- Fatty or fried foods: Slow digestion, keep the LES opened longer.
- Spicy seasonings: Irritate the esophageal lining and boost acid production.
- Caffeine & carbonated drinks: Relax the LES and add gas.
- Alcohol: Weakens LES tone and inflames the stomach lining.
- Late‑night eating: Lying down makes it easier for acid to flow upward.
- Stress: Triggers hormonal changes that increase stomach acid and heighten pain perception.
Notice how many of these are lifestyle choices rather than mysterious medical conditions. That’s why simple adjustments can often calm both the burn and the ache.
How Gastroesophageal Reflux Disease (GERD) a chronic form of acid reflux that occurs at least twice a week fits in
If heartburn shows up more than a few times a month, doctors may label it GERD. GERD isn’t just an occasional flare‑up; it means the LES is persistently lax, exposing the esophagus to acid for long periods. Over time, that can lead to inflammation, ulcers, or even Barrett’s esophagus-a precancerous change.
People with GERD often report a lingering tummy ache because the same acid irritation can cause the stomach lining to become sensitive. Moreover, chronic reflux can slow gastric emptying, creating a feedback loop of pressure, reflux, and abdominal discomfort.
Quick dietary tweaks for dual relief
Changing what you put on your plate can hit two birds with one stone. Try these evidence‑backed moves:
- Eat smaller, more frequent meals. Think 5‑6 mini‑plates instead of three giant ones.
- Stay upright for at least 30 minutes after eating. Sitting or standing keeps gravity on your side.
- Swap citrus and tomato‑based sauces for milder herbs (basil, oregano, ginger).
- Limit caffeine to one cup a day and choose low‑acid coffee or tea.
- Replace fizzy sodas with still water or herbal teas; mint tea can soothe the stomach, but avoid peppermint if you have reflux.
- Introduce a handful of almonds after meals; healthy fats help close the LES.
- Chew gum (sugar‑free) for 20 minutes post‑meal; increased saliva neutralizes acid.
These changes target the LES and stomach pressure simultaneously, meaning less burning and fewer belly cramps.
When over‑the‑counter isn’t enough
Antacids (like calcium carbonate) neutralize acid quickly and are handy for an occasional heartburn flare. However, they don’t address the underlying LES weakness, nor do they relieve a tummy ache caused by gas, ulcer, or inflammation.
H2 blockers (e.g., ranitidine alternatives) and PPIs (proton‑pump inhibitors) reduce acid production and can help both conditions, but long‑term use should be discussed with a physician because they may affect nutrient absorption.
If you suspect a peptic ulcer a sore on the stomach lining caused by excess acid or H. pylori infection, antacids alone won’t heal it. You’ll need a proper diagnosis and possibly antibiotics or targeted medication.
Lifestyle habits beyond food
Stress management is a silent hero. When you’re anxious, your body releases cortisol, which can increase stomach acid and heighten pain perception. Simple practices-deep breathing, 10‑minute walks, or a short meditation-can lower stress hormones and keep the LES tighter.
Physical activity also matters. Regular moderate exercise (like brisk walking or cycling) promotes healthy digestion and weight management. Extra weight, especially around the abdomen, pushes up on the stomach and forces the LES open.
Sleep positioning is another hidden trick. Elevating the head of your bed by 6‑8 inches (or using a wedge pillow) uses gravity to keep acid where it belongs while you snooze.
Red flags: when to book a doctor’s visit
Most heartburn and tummy aches are benign, but some signs signal a deeper issue:
- Chest pain that radiates to the arm or jaw (could be cardiac).
- Vomiting blood or material that looks like coffee grounds.
- Unintended weight loss or loss of appetite.
- Pain that wakes you up at night consistently.
- Difficulty swallowing or feeling of food stuck in the throat.
If any of these appear, schedule a medical appointment ASAP. Tests like an upper endoscopy or barium swallow can pinpoint ulcers, strictures, or severe GERD.
Comparison: Common triggers for heartburn vs. tummy ache
| Trigger | Heartburn | Tummy Ache |
|---|---|---|
| Large meals | Often provokes reflux by raising stomach pressure | Can overstretch the stomach, causing cramping |
| Spicy foods | Irritates esophageal lining, increases acid | May cause gastric irritation and gas |
| Caffeine | Relaxes LES, allowing acid back‑flow | Stimulates gastric acid, can lead to discomfort |
| Stress | Boosts acid production, lowers LES tone | Alters gut motility, leading to bloating |
| Alcohol | Weakens LES and irritates esophagus | Can inflame gastric mucosa, causing pain |
Putting it all together: a 3‑day relief plan
Here’s a simple roadmap you can start tonight:
- Day 1 - Clean reset: Skip heavy meals after 7pm, drink only water or herbal tea. Take an OTC antacid if you feel a burn.
- Day 2 - Gentle nutrition: Breakfast oatmeal with banana, lunch salad with lean protein, dinner baked fish + steamed veggies. Chew each bite 20‑30 times.
- Day 3 - Lifestyle lock‑in: Add a 15‑minute evening walk, practice 5‑minute deep‑breathing before bed, and raise your head of the bed.
If symptoms improve, keep the habits. If not, it’s time to see a clinician for possible GERD testing.

Frequently Asked Questions
Can heartburn cause a real stomach ulcer?
Heartburn itself isn’t a direct cause of ulcers, but chronic acid exposure can damage the stomach lining over time, especially if you also have H.pylori infection or regularly use NSAIDs. If you notice persistent pain, get tested.
Why does lying down make my heartburn worse?
When you lie flat, gravity no longer helps keep stomach acid down. The LES has to work harder, and any weakness lets acid travel upward, sparking that burning feeling.
Are antacids safe to use every day?
Occasional use is fine, but daily reliance can lead to electrolyte imbalances and affect calcium absorption. Talk to a doctor about stronger, longer‑term options if you need daily relief.
What foods should I avoid if I get both heartburn and tummy ache?
Stick away from fried foods, chocolate, citrus, tomato sauces, caffeine, carbonated drinks, and large meals late at night. These are the top triggers for both symptoms.
When is it time to get an endoscopy?
If you have frequent heartburn (more than twice a week), unexplained weight loss, vomiting blood, or pain that wakes you at night, a doctor will likely suggest an upper endoscopy to check for erosive esophagitis, Barrett’s, or ulcers.
Brian Mavigliano
September 30, 2025 AT 21:51Ah, the age‑old dance of fire‑kissed esophagus and rumbling belly – a duet most mortals mistake for mere indigestion. Yet, beneath the banal veneer lies a cosmic paradox: the very fire that scorches the throat also fuels the churn of the gut. One might argue that our bodies are staging a rebellion against the very foods we worship. In that sense, heartburn and tummy ache are not symptoms, but philosophical protest signs.
Emily Torbert
October 8, 2025 AT 13:51i totally get how uncomfortable that can be its like your body is sending a tiny SOS and you just want it to stop i think the little tweaks like smaller meals and not lying down right after can really help
Rashi Shetty
October 16, 2025 AT 05:51Dear reader, it is incumbent upon us to reflect upon the moral dimensions of our dietary choices. The consumption of excessively spicy or fatty fare is not merely a personal indulgence but a transgression against the sanctity of one's internal equilibrium. One must recognize that the LES, that humble sphincter, is a guardian of physiological virtue. When we jeopardize its function, we invite the ignominy of acid reflux and the accompanying visceral lament. Moreover, the prevalence of stress as a catalyst is a testament to the interconnectedness of mind and body. 🌿 It is, therefore, imperative to adopt a regimen of moderation, mindfulness, and respect for the corporeal temple. Neglecting these principles may lead to chronic ailments such as GERD, which, beyond discomfort, carries the specter of severe complications. Let us, as custodians of our own health, eschew the reckless excesses that precipitate both heartburn and abdominal distress. 🍎 The path to relief is paved with conscious decisions, balanced nutrition, and disciplined lifestyle practices. May we all strive toward that enlightened state of gastrointestinal harmony.
Queen Flipcharts
October 23, 2025 AT 21:51While the discourse above flutters in abstract nuance, let us be unequivocal: the United States, whose culinary heritage champions hearty portions, must lead by example in championing restraint. A nation that reveres liberty must also honor the liberty of its digestive tract from the tyranny of acid. By adopting prudent eating customs, we safeguard not only individual health but the vigor of our great republic.
Yojana Geete
October 31, 2025 AT 12:51O majestic audience, behold the tragedy! The very act of savoring a midnight pizza becomes an operatic catastrophe, a drama of fire and ache. Yet, in the hush of your cravings lies the silent whisper of a LES pleading for mercy. Let us not be mere spectators but protagonists who command our plates with regal poise.
Jason Peart
November 8, 2025 AT 04:51Hey there! I totally feel you – those late‑night bites can feel like a betrayal. Remember, buddy, chew each bite like you’re savouring a story, and try a quick walk after dinner – it works wonders. Also, keep a water bottle handy; staying hydrated can soothe the fire and calm the tummy.
Hanna Sundqvist
November 15, 2025 AT 20:51Listen, they don’t tell you in the magazines that the real cause is the hidden agenda of food corporations pushing us to overeat. It's all designed to keep the LES weak so we buy more antacids, keeping us dependent. Wake up, question the narrative, and take control of your digestion.
Jim Butler
November 23, 2025 AT 12:51Stand tall, dear friends! Your bodies are capable of reclaiming balance – choose mindful meals, elevate your head, and breathe deeply. 🌟 Together we rise above the burn and the ache! 💪😊
Ian McKay
December 1, 2025 AT 04:51Additionally, your sentence "they dont" should be "they don't".
Deborah Messick
December 8, 2025 AT 20:51It is a curious folly that one would dismiss the profound ethical implications of habitual overindulgence; such negligence borders on moral irresponsibility. While others celebrate convenience, we must uphold the higher standard of disciplined nourishment.