DDAVP Spray vs Alternatives: Desmopressin Comparison Guide
 Oct, 20 2025
Oct, 20 2025
Bedwetting Treatment Recommender
Your Treatment Preferences
Treatment Options Comparison
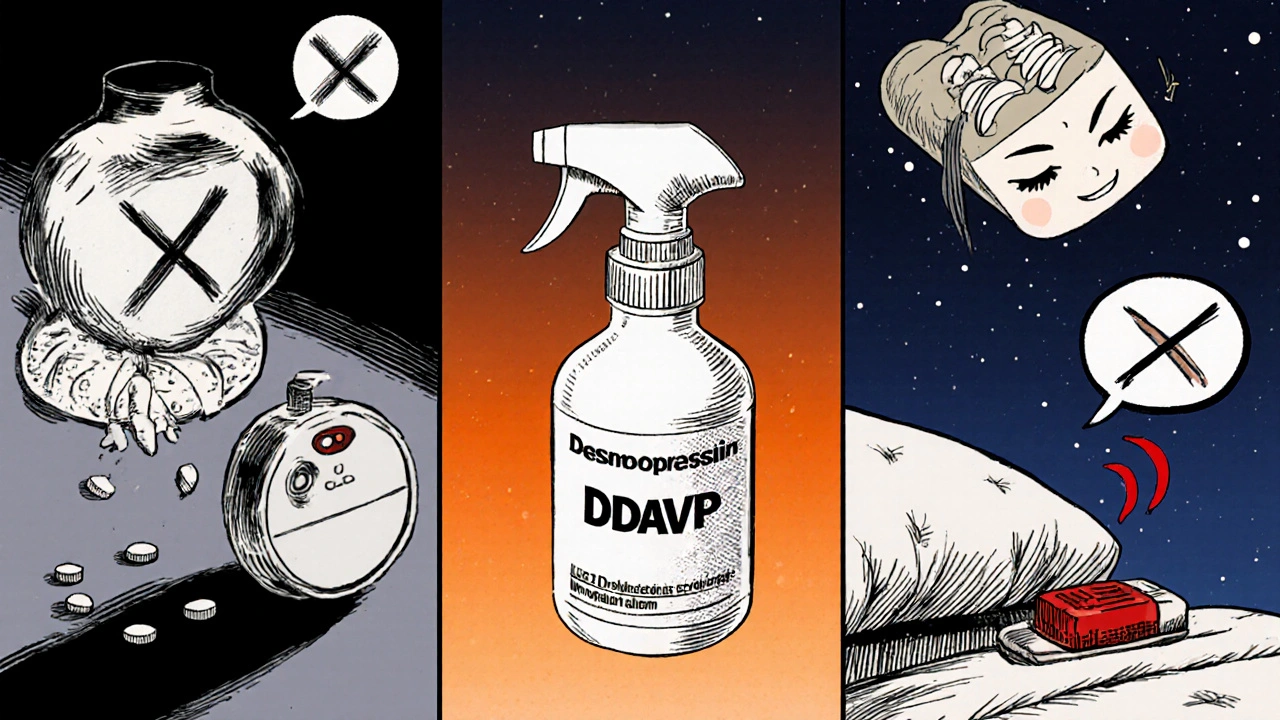
DDAVP Nasal Spray
Fast onsetReduces wet nights by 55-70% with 30-45 min onset. Best for rapid control when fluid restrictions can be followed.
Bedwetting Alarm
No side effectsBuilds lasting bladder control with 40-70% long-term reduction. Requires commitment to training but no medications.
Desmopressin Tablets
Slower onsetSimilar effects to spray but 60-90 min onset. Good option if nasal irritation is a concern.
Quick Takeaways
- DDAVP spray is a nasal form of desmopressin acetate that works fast for night‑time bedwetting.
- Oral desmopressin tablets give similar hormone effects but have a slower onset.
- Alarm therapy has no drug side‑effects and builds lasting bladder control.
- Imipramine and methylphenidate can help, but they bring cardiovascular and appetite‑suppression concerns.
- Cost, dosing convenience, and risk of low sodium (hyponatremia) often decide the best choice.
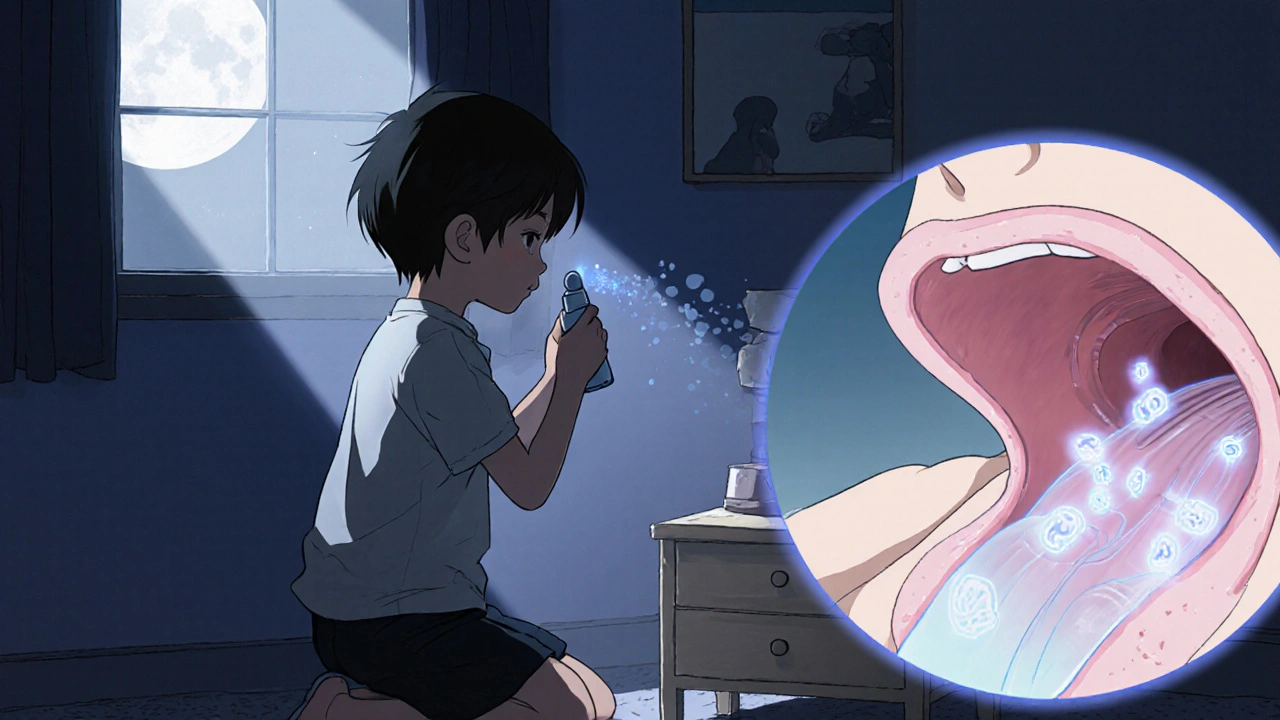
What is DDAVP Spray?
DDAVP spray is a desmopressin acetate nasal spray used to treat nocturnal enuresis and certain bleeding disorders. The spray delivers a synthetic version of the hormone vasopressin directly to the bloodstream via the nasal mucosa, bypassing the gut. This rapid absorption makes it popular for kids and adults who need quick control of nighttime urine production.
Desmopressin acetate mimics the antidiuretic hormone (ADH) that tells the kidneys to re‑absorb water, reducing the volume of urine formed during sleep. For many users, a single spray before bedtime can cut night‑time wetting episodes by more than half.
How Does DDAVP Spray Work?
The active molecule binds to V2 receptors in the kidney’s collecting ducts. That triggers a cascade that inserts aquaporin‑2 water channels into the duct walls, allowing water to be pulled back into the bloodstream instead of being excreted. The effect peaks within 30-45 minutes and lasts about 8‑10 hours, which aligns well with typical sleep cycles.
Because the spray avoids first‑pass metabolism, the required dose is lower than oral tablets-usually 0.1 mg per spray for children and 0.2 mg for adults. Lower dosing means a slightly reduced risk of water retention, but the danger of hyponatremia (low blood sodium) still exists, especially if fluid intake isn’t limited.
Alternatives Overview
People who can’t tolerate the spray or who prefer a non‑pharmacologic route have several options:
- Desmopressin tablets (often sold as Minirin) - oral form, slower onset, same hormone effect.
- Methylphenidate - a stimulant used off‑label for bedwetting; works by increasing bladder capacity through central nervous system activation.
- Imipramine - a tricyclic antidepressant that relaxes the sphincter and raises the sleep arousal threshold.
- Bedwetting alarm - a device that sounds when moisture is detected, training the brain to wake up before a full bladder.
- Tolterodine - an anticholinergic sometimes prescribed for overactive bladder, used off‑label for refractory enuresis.
Comparing Efficacy
| Option | Typical Reduction in Wet Nights (%) | Onset Time | Duration of Effect |
|---|---|---|---|
| DDAVP spray | 55‑70 | 30‑45 min | 8‑10 h |
| Desmopressin tablets (Minirin) | 45‑60 | 60‑90 min | 10‑12 h |
| Methylphenidate | 30‑50 | 45‑60 min | 6‑8 h |
| Imipramine | 35‑55 | 1‑2 h | 12‑14 h |
| Bedwetting alarm | 40‑70 (long‑term) | Immediate (behavioral) | Continues until habit breaks |
Notice how the spray tops the short‑term reduction chart, but the alarm catches up (and often surpasses) once the child learns to wake up on a full bladder. For families that want a quick fix, the spray or tablets are attractive; for lasting habit change, the alarm shines.
Safety & Side‑Effect Profile
All options carry some risk. Here’s a quick snapshot:
- DDAVP spray: most common issues are mild nasal irritation and hyponatremia if fluid restriction isn’t followed.
- Desmopressin tablets: similar hyponatremia risk, plus occasional GI upset.
- Methylphenidate: appetite loss, insomnia, and a small increase in heart rate.
- Imipramine: dry mouth, constipation, and, rarely, cardiac conduction changes.
- Bedwetting alarm: skin irritation from the sensor and possible sleep disruption during the training period.
- Tolterodine: dry mouth, blurred vision, and potential constipation.
Hyponatremia is the biggest red flag for any desmopressin product. Blood sodium should be checked after the first few nights, especially for kids under 10 or for adults with heart/kidney disease.
Practical Considerations: Cost, Convenience, and Compliance
Cost varies by country and insurance coverage. In New Zealand, a pack of DDAVP spray (10 sprays) runs around NZ$30, while oral tablets are slightly cheaper at NZ$20 for a month’s supply. Alarm devices cost NZ$70‑$120 but are a one‑time purchase.
Convenience matters: the spray only needs a quick puff before bedtime-perfect for families with chaotic evenings. Tablets require swallowing, which some kids dislike. Alarms need a sensor to stay attached to the mattress and may wake the whole household during the learning phase.
Compliance is the biggest predictor of success. If a child hates the taste of tablets, the spray wins. If the family finds alarms too noisy, medication may be the fallback.
Choosing the Right Option for Your Situation
Ask yourself these three questions:
- Do I need rapid symptom control or a long‑term habit change?
- Is the child able to follow fluid‑restriction advice safely?
- What budget constraints or insurance coverage do I have?
If fast control is the goal and fluid restriction can be managed, DDAVP spray is often the first‑line pick. If you’re looking for a drug‑free solution and have patience for a few weeks of training, the bedwetting alarm may be the smarter investment.
For children who haven’t responded to either spray or alarm, a trial of methylphenidate or imipramine under pediatric supervision becomes reasonable. Always weigh cardiovascular side‑effects (especially with methylphenidate) against the modest extra benefit.
Key Takeaway Checklist
- DDAVP spray offers the fastest onset and strong short‑term reduction.
- Oral desmopressin works similarly but slower; choose if nasal irritation is a concern.
- Alarms provide lasting habit‑forming results without medication risks.
- Stimulants and tricyclics can help refractory cases but demand careful monitoring.
- Check sodium levels early; educate the whole household about fluid limits.
Frequently Asked Questions
How long should I use DDAVP spray?
Most clinicians recommend a trial of 4‑6 weeks. If bedtime wetting improves by at least 50 %, a gradual taper is advised to avoid rebound wetting. Long‑term use is possible but requires regular sodium monitoring.
Can adults use DDAVP spray for bedwetting?
Yes. Adults with nocturnal enuresis often benefit, but dosage adjustments are needed because adult kidneys handle water differently. A physician should start with a low dose and watch for hyponatremia.
Is the alarm therapy covered by insurance?
Coverage varies by provider. In New Zealand’s public health system, the alarm is usually classified as a medical device and may be subsidised if prescribed by a pediatrician.
What fluid restrictions should I follow?
Limit drinks to 500 ml after the evening dose and avoid sports drinks or soda that are high in sodium. Encourage a normal water intake earlier in the day to keep overall hydration adequate.
Are there any drug interactions with DDAVP spray?
Yes. NSAIDs, certain antidepressants (SSRIs), and carbamazepine can increase the risk of hyponatremia. Always list all current meds to your prescriber before starting desmopressin.
jessie cole
October 20, 2025 AT 20:45I commend the thoroughness of this guide; it offers a clear path for families navigating nocturnal enuresis. The distinction between rapid‑acting DDAVP spray and slower oral tablets is articulated with precision. Parents will appreciate the emphasis on fluid restriction to mitigate hyponatremia, a prudent safety measure. Moreover, the inclusion of non‑pharmacologic alarm therapy highlights a balanced approach. Ultimately, the checklist at the end serves as an excellent reference for making informed decisions.
Kirsten Youtsey
October 22, 2025 AT 00:31One cannot help but notice that the article glosses over the pharmaceutical industry's hidden motives. The author conveniently omits the fact that DDAVP spray is a revenue stream for certain conglomerates eager to keep patients dependent. While the guide mentions side‑effects, it fails to question the long‑term ecological impact of manufacturing synthetic vasopressin. In truth, the simplest solution-behavioral training-remains undervalued because it does not line anyone’s pockets.
Ron Lanham
October 23, 2025 AT 04:18The pharmacodynamics of desmopressin, whether delivered nasally or orally, deserve a nuanced discussion that extends beyond simple efficacy percentages.
First, the rapid absorption of the nasal spray bypasses hepatic metabolism, thereby reducing the required dose to achieve antidiuretic effect.
Second, this lower dose mitigates, though does not eliminate, the risk of water retention that can precipitate hyponatremia.
Third, the timing of administration-typically 30 minutes before bedtime-aligns neatly with the circadian rhythm of nocturnal urine production.
Fourth, the nasal mucosa can be a source of irritation, which may diminish adherence in younger patients prone to sensory sensitivities.
Fifth, the oral tablet formulation, while slower to act, offers the advantage of precise dosing through split tablets, a feature the spray lacks.
Sixth, the tablet's longer duration of action can be beneficial for extended sleep periods but may increase the window for potential electrolyte disturbances.
Seventh, the comparative cost analysis must factor in insurance formularies, as some plans cover tablets but deem nasal sprays as specialty items.
Eighth, the behavioral alarm, though drug‑free, imposes a psychological burden that can affect sleep quality during the training phase.
Ninth, stimulant therapy such as methylphenidate introduces cardiovascular considerations that are irrelevant for desmopressin but cannot be ignored in a holistic treatment plan.
Tenth, tricyclic agents like imipramine carry anticholinergic side effects, a stark contrast to the relatively clean side‑effect profile of desmopressin when used responsibly.
Eleventh, the clinician must weigh parental preference for convenience against the child’s willingness to tolerate nasal administration.
Twelfth, fluid restriction protocols should be individualized; a blanket 500 ml limit may be too restrictive for active adolescents.
Thirteenth, regular monitoring of serum sodium is non‑negotiable during the initial weeks, especially in patients with concurrent renal or cardiac disease.
Finally, a shared decision‑making model that presents these variables transparently empowers families to choose the option that best aligns with their lifestyle and safety priorities.
Andrew Hernandez
October 24, 2025 AT 08:05Punctual compliance with fluid restriction remains the cornerstone of safe DDAVP use.
Alex Pegg
October 25, 2025 AT 11:51While many hail the spray as a miracle, the real patriot‑born solution lies in self‑reliance: teach the child to wake naturally without pharmaceutical crutches. The alarm, though noisy, fosters independence and avoids foreign chemical dependence. Moreover, relying on a US‑manufactured nasal spray makes families vulnerable to supply chain disruptions. A resilient family chooses habit over hype.
JessicaAnn Sutton
October 26, 2025 AT 14:38The guide, albeit comprehensive, suffers from a lack of quantitative risk stratification for hyponatremia. Precise thresholds-serum sodium < 130 mmol/L-should be mandated before continuation. Additionally, the cost comparison omits pharmacy dispensing fees which can double the expense of spray therapy. A more rigorous citation of peer‑reviewed studies would bolster credibility. Until then, readers must interpret the recommendations with scholarly caution.
Israel Emory
October 27, 2025 AT 18:25It is commendable that the article presents both pharmacologic and behavioral options; this balance respects diverse family values. Fluid restriction, however, should be individualized rather than prescribed as a blanket rule. Parents might consider a gradual reduction strategy to minimize disruption. Open dialogue with a pediatrician remains essential for safe implementation.
Sebastian Green
October 28, 2025 AT 22:11I understand how overwhelming these choices can feel; many families share that sentiment. Remember that consistency, no matter the method, often yields the best outcomes.
Wesley Humble
October 30, 2025 AT 01:58Statistically, the spray achieves a 62 % reduction in wet nights, outperforming tablets by a modest 5 % margin. 📊 Yet, the incidence of hyponatremia rises from 1 % to 3 % when fluid restriction is ignored. ⚠️ The alarm, while slower to show results, demonstrates a 70 % long‑term success rate without pharmacologic risk. 🛎️ Consequently, a cost‑benefit analysis should weigh immediate efficacy against potential electrolyte disturbance. 📈