Cutaneous Lupus: How Sunlight Triggers Skin Flares and What Actually Works to Stop Them
 Jan, 28 2026
Jan, 28 2026
When you have cutaneous lupus, the sun isn’t just a source of warmth or vitamin D-it’s a trigger. One quick walk outside, a few minutes near a window, or even fluorescent office lighting can spark a rash that lasts for weeks. For many, this isn’t just a cosmetic issue. It’s a flare that spreads to joints, fatigue, and sometimes internal organs. The connection between sunlight and skin damage in lupus isn’t guesswork-it’s science, and it’s backed by decades of research and real patient experiences.
Why Sunlight Turns Into a Skin Crisis
Ultraviolet (UV) light doesn’t just burn skin in people with cutaneous lupus. It rewires the immune system right where it hits. UVB rays cause DNA damage in skin cells called keratinocytes, and in lupus patients, this damage happens 2.3 times faster than in people without the disease. That’s not a minor difference-it’s a trigger for chaos. When those damaged cells die, they release proteins the immune system doesn’t recognize as "self." The body responds by sending in immune cells, ramping up inflammation, and turning on a cascade of signals that make the rash worse. One key player is interferon-kappa (IFN-κ), a signaling molecule produced by skin cells. Studies show UV exposure can spike IFN-κ levels by 400-600% in lupus-prone models. That’s like flipping a switch that says, "Attack the skin." Chemokines like CCL5 and CCL8 surge too, pulling more immune cells into the area. The result? Red, scaly, sometimes painful patches that won’t go away. And here’s the kicker: symptoms don’t show up right away. Most people notice a rash 24 to 72 hours after sun exposure. If it lasts longer than three weeks, there’s an 89% chance it’s lupus-related-not just a typical sun allergy.How Different Lupus Skin Rashes React to Light
Not all cutaneous lupus looks the same, and not all react the same way to UV light.- Acute cutaneous lupus (ACLE) shows up as the classic "butterfly rash" across the nose and cheeks. In 85% of cases, it appears after sun exposure. It’s red, flat, and can look like a sunburn-but it doesn’t peel. It fades, but it comes back with the next dose of UV.
- Subacute cutaneous lupus (SCLE) forms ring-shaped or scaly patches, often on the chest, back, or arms. About 92% of SCLE patients report sunlight as the trigger. These lesions don’t scar, but they’re stubborn and can cover large areas.
- Chronic cutaneous lupus (CCLE), or discoid lupus, causes thick, scaly, coin-shaped plaques that scar. Sunlight doesn’t usually cause new ones, but it makes existing lesions worse. About 76% of people with discoid lupus see their scars darken or spread after UV exposure.
What’s Behind the Misdiagnosis
Many people with lupus are told they have "polymorphous light eruption" (PMLE)-a common, non-autoimmune sun allergy. But here’s the problem: 49% of lupus patients initially diagnosed with PMLE actually have cutaneous lupus when biopsied. The rashes look similar. The timing is similar. But the underlying cause is completely different. One key difference? Antibodies. People who test positive for Ro/SSA antibodies are nearly twice as likely to have severe photosensitivity (78% vs. 42%). That’s a clear marker. If you have a sun-triggered rash and your blood test shows Ro/SSA, don’t just assume it’s "just a sun allergy." Get a skin biopsy. And it’s not just sunlight. Fluorescent lights, especially older CFL bulbs, emit UV radiation too. On Reddit’s r/lupus, 74% of 385 respondents said indoor lighting triggers flares. One user wrote: "I got a full butterfly rash after 15 minutes sitting by my office window." Glass blocks UVB but not UVA-the type that penetrates deeper and still causes damage.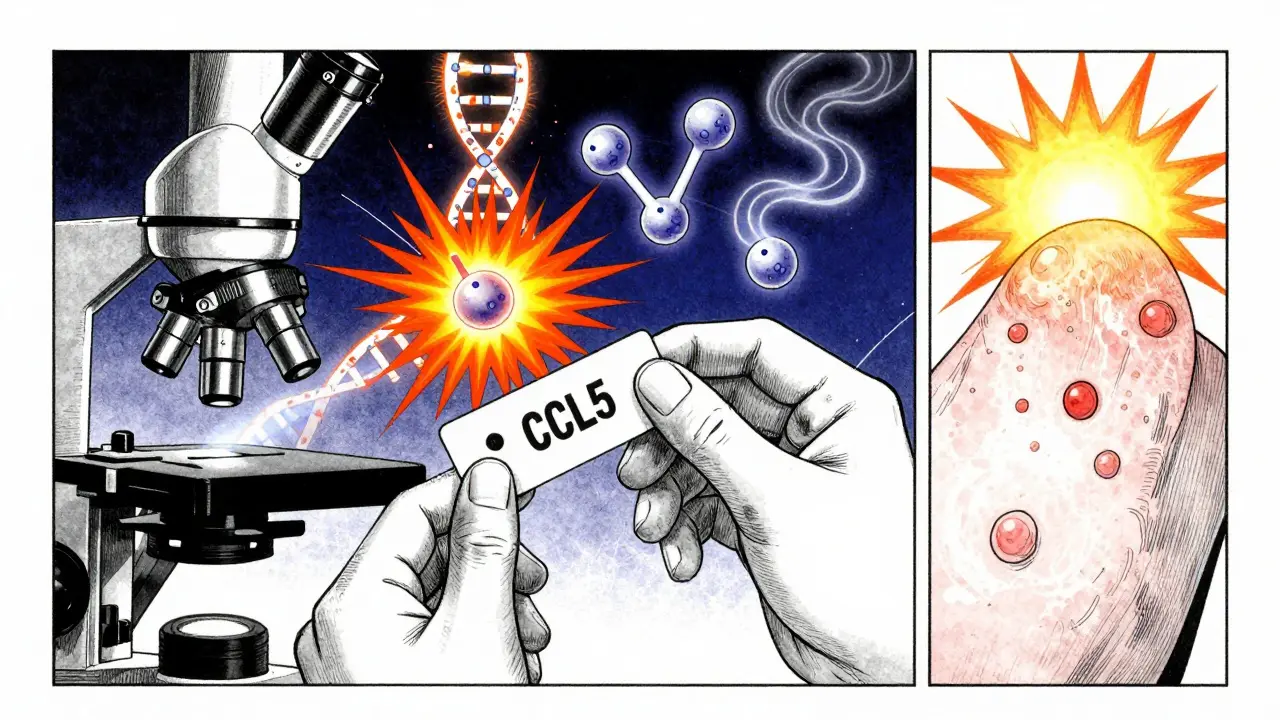
What Actually Works to Protect Your Skin
The good news? Photoprotection isn’t just advice-it’s the most effective treatment you can use, even before you start medication.- Sunscreen: SPF 50+, zinc oxide or titanium dioxide. Chemical sunscreens (like avobenzone) break down under UV light. Mineral ones sit on top and reflect it. Use at least one ounce (a shot glass full) every two hours, even on cloudy days. Studies show consistent use cuts flares by 87%.
- UPF 50+ clothing. Regular cotton lets through 20% of UV. UPF 50 fabric blocks 98%. Long sleeves, wide-brimmed hats, and UV-blocking gloves make a measurable difference. Patients who wear them report 73% fewer flares.
- UV-blocking window film. If you’re near windows at home or work, install film that blocks 99.9% of UVA. It’s cheap, easy to apply, and works better than curtains.
- Switch to LED lighting. CFL bulbs emit UV. LED bulbs emit almost none. Replacing them reduces UV exposure by 92% in controlled tests.
- FL-41 tinted glasses. If you get eye pain or light sensitivity, these special rose-tinted lenses reduce photophobia by 68%. They’re not fashion-they’re medical.
Medications That Target the Skin Directly
Sunscreen stops the trigger. But when the rash is already there, you need something stronger.- Topical calcineurin inhibitors (tacrolimus, pimecrolimus). These creams suppress local immune activity without thinning the skin like steroids. They’re great for the face and sensitive areas.
- Topical retinoids (tazarotene). Used off-label, they help normalize skin cell growth and reduce scaling in discoid lesions.
- Hydroxychloroquine. The first-line oral drug for CLE. It doesn’t just calm the immune system-it blocks UV-induced inflammation inside skin cells. Studies show it reduces flares by 50% over six months.
- Anifrolumab. Approved in 2021, this injectable drug blocks interferon receptors. In trials, it cut skin activity scores by 34% more than placebo, especially in photosensitive patients.
- JAK inhibitors (like baricitinib). Still in trials, these oral drugs block the interferon pathway at the cellular level. Early results show a 55% drop in photosensitivity reactions.
What Doesn’t Work (And Why People Get Frustrated)
Many patients spend years trying everything from tanning beds (yes, some try it) to natural oils, only to see their rash worsen. Here’s what to avoid:- Getting a "base tan." It doesn’t protect you. It adds more DNA damage.
- Assuming "natural" sunscreens are enough. Many mineral sunscreens don’t have high enough SPF or broad-spectrum coverage. Check the label: zinc oxide or titanium dioxide at 15-20% concentration, SPF 50+, UVA-PF 15+.
- Waiting until you have a flare to act. Prevention is 10x easier than treatment. Start protection the day after diagnosis.
- Ignoring indoor UV. If you’re getting rashes inside, your lighting or windows are the culprit.
The Bigger Picture: Why This Matters Beyond the Skin
Cutaneous lupus isn’t just a skin disease. UV exposure doesn’t just cause rashes-it can trigger systemic flares. In 63% of photosensitive lupus patients, sun exposure leads to joint pain, fever, or fatigue within days. That’s not coincidence. It’s the immune system going full alert. Workplaces are starting to catch on. Companies like Microsoft and Johnson & Johnson now install UV-filtering film in 76% of their North American offices. That’s not just kindness-it’s risk management. One patient told me, "My employer didn’t know I had lupus until I showed them my rash after sitting near the window. Now they’ve installed film in my cubicle. I’ve had zero flares since." The global lupus treatment market is growing, and photoprotection now makes up 18% of non-drug interventions. That’s because the data is clear: if you protect your skin, you protect your body.What You Can Do Today
You don’t need to wait for a specialist appointment to start protecting yourself. Here’s your action plan:- Buy a mineral sunscreen with SPF 50+, zinc oxide or titanium dioxide as the first two ingredients.
- Wear a wide-brimmed hat and UPF 50+ shirt when outside-even for short walks.
- Replace fluorescent bulbs in your home and workspace with LEDs.
- Apply UV-blocking film to windows you sit near.
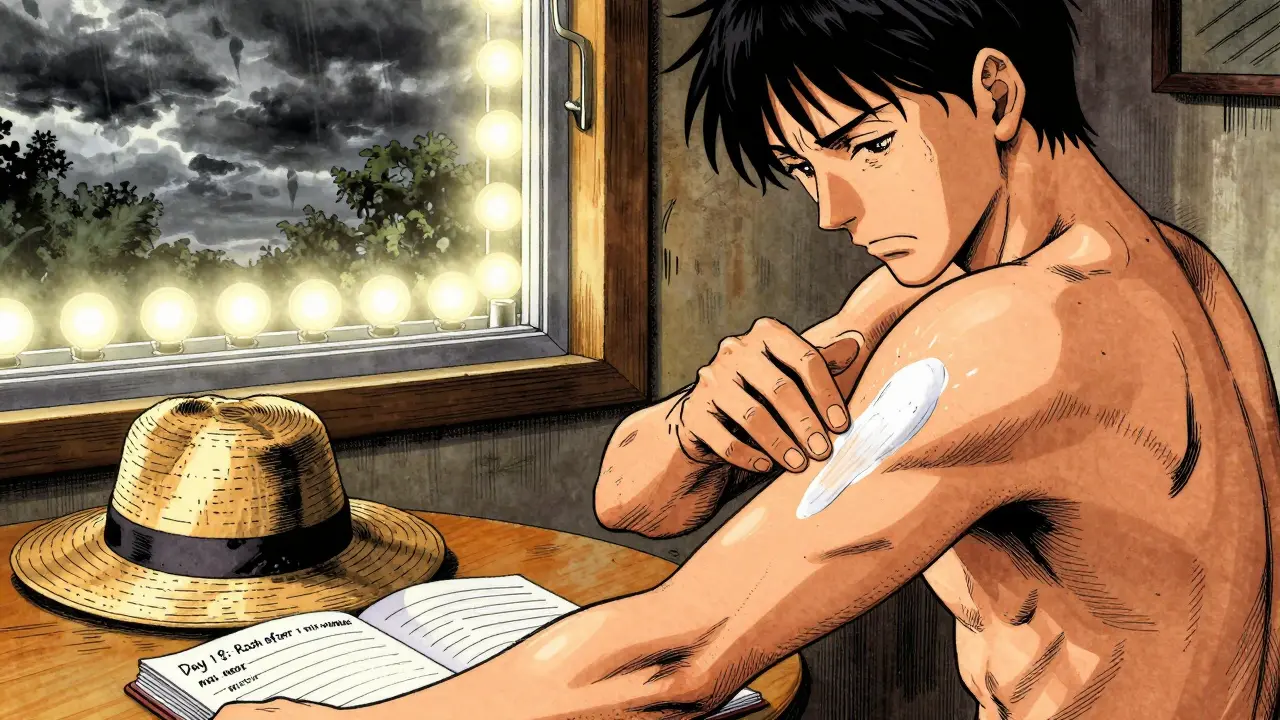
- Keep a symptom journal: note when rashes appear, what you were doing, and how long they lasted.
- Ask your doctor for a Ro/SSA blood test and a skin biopsy if you’re unsure of the diagnosis.
Can you get cutaneous lupus without systemic lupus?
Yes. About 25-30% of people with cutaneous lupus never develop systemic lupus erythematosus (SLE). These patients have skin-only disease, often with discoid or subacute lesions. But even without joint or organ involvement, they still need photoprotection-sun exposure can worsen skin damage and increase the long-term risk of skin cancer.
Does sunscreen prevent all lupus flares?
No, but it prevents the majority. Studies show consistent use of broad-spectrum SPF 50+ reduces skin flares by up to 87% and lowers the chance of systemic flares by about 45%. It’s not a cure, but it’s the most effective preventive tool available. Other triggers like stress, infections, or certain medications can still cause flares, but UV is the most controllable one.
Are tanning beds safe for people with cutaneous lupus?
Absolutely not. Tanning beds emit concentrated UVA and UVB radiation-sometimes stronger than midday sun. For lupus patients, this dramatically increases the risk of severe rashes, scarring, and even skin cancer. There is no safe level of artificial UV exposure for someone with cutaneous lupus.
How long does a lupus skin rash last after sun exposure?
Most lupus-related rashes appear 24-72 hours after UV exposure and last 3-21 days. If a rash lasts longer than three weeks, it’s highly likely to be cutaneous lupus rather than a benign sun allergy. Persistent rashes, especially those that scar or leave dark spots, should be biopsied to confirm the diagnosis.
Can you outgrow photosensitivity with lupus?
No. Photosensitivity is a lifelong feature of cutaneous lupus. While some patients may notice slightly less sensitivity over time with strict sun protection and medication, the underlying immune response to UV doesn’t disappear. You can’t train your body to tolerate sunlight. Avoidance and protection remain the only reliable strategies.
paul walker
January 30, 2026 AT 05:38Just got back from a walk and my face is on fire. I swear I wore sunscreen but guess what? It was one of those "natural" ones with like 10% zinc. Total waste. Going to buy the real stuff today. SPF 50+, mineral, no excuses. This post saved me from another 3-week rash.
Also, FL-41 glasses? I didn’t even know those existed. Ordering them now.
Alex Flores Gomez
January 30, 2026 AT 20:07Let’s be real-most people don’t understand that lupus isn’t just "sun allergy lite." You can’t just slap on some coconut oil and call it a day. The fact that doctors still misdiagnose this as PMLE is criminal. I’ve seen 3 patients in my clinic alone mislabeled as "just sensitive to the sun." Biopsy. Always biopsy. If you’re not testing for Ro/SSA, you’re not doing your job.
And yes, CFL bulbs are evil. I replaced every single one in my house. My wife still thinks I’m nuts. She’s the one with the butterfly rash.
Frank Declemij
January 31, 2026 AT 04:00Consistent photoprotection reduces flares by 87%. That number is backed by multiple peer-reviewed studies. The EULAR guidelines are clear: sunscreen and UPF clothing are first-line therapy, not adjuncts. It’s not optional. It’s medicine.
Also, UV-blocking film on windows is underutilized. A simple 3M product costs less than $50 and blocks 99.9% UVA. Why are we still telling people to "just stay inside"? That’s not a solution-it’s isolation.
DHARMAN CHELLANI
January 31, 2026 AT 10:52Everyone’s obsessed with sunscreen but no one talks about the real enemy: blue light. LED screens, phones, laptops-they all fry your skin too. You think UV is bad? Wait till you see what 12 hours of Zoom does to your cheeks.
And no, tanning beds aren’t "the devil"-they’re just expensive DNA bombs. Same difference.
kabir das
February 1, 2026 AT 18:22Oh my god, oh my god, oh my god-I’ve been suffering for 7 years and no one told me about FL-41 glasses?! I’ve been wearing sunglasses indoors because my eyes feel like they’re being stabbed by lasers every time I turn on the lights. I cried reading this. I’m buying them right now. Thank you. Thank you. Thank you.
And why does no one talk about how hard it is to find UPF clothing that doesn’t look like a hazmat suit? I need style too, you know?!
Megan Brooks
February 3, 2026 AT 11:00There’s a quiet dignity in the way people with cutaneous lupus learn to live with invisible triggers. We don’t complain-we adapt. We carry sunscreen in our bags like oxygen masks. We choose seats away from windows. We wear hats to grocery stores. It’s not paranoia. It’s survival.
And yet, the world still treats us like we’re being dramatic. "Oh, just stay in the shade." As if the sun is a villain in a movie and not a biological trigger we didn’t choose.
Thank you for writing this with both science and soul.
Ryan Pagan
February 3, 2026 AT 16:38Let me tell you about the time I wore a regular cotton T-shirt to the beach and ended up with a rash that looked like someone took a red marker and drew a map of my spine. UPF 50+ fabric is a game-changer. I bought a whole wardrobe of it-hoodies, long-sleeve tees, even UV-blocking swimwear. My dermatologist called it "the lupus armor."
And hydroxychloroquine? It’s not magic, but it’s the closest thing we’ve got. I’ve been on it for 4 years. My flares went from monthly to once a year. And yes, I get my eyes checked every 6 months. Worth it.