Bronchial Asthma vs COPD: Key Differences Explained
 Oct, 23 2025
Oct, 23 2025
Asthma vs COPD Diagnostic Calculator
How This Tool Works
This calculator helps you understand how spirometry results can determine if you have asthma or COPD. The key difference is reversibility: asthma shows significant improvement after bronchodilators while COPD does not. Enter your pre- and post-bronchodilator measurements to see if your results indicate asthma or COPD.
Enter Your Spirometry Results
Ever wonder why two people with shortness of breath can get such different diagnoses? One might be told they have asthma, the other COPD, yet both sound like they’re struggling to catch their breath. The truth is, these conditions share a few symptoms but diverge dramatically in cause, progression, and treatment. This guide pulls apart the medical jargon so you can see where the lines are drawn and, more importantly, what that means for daily life.
Key Takeaways
- Bronchial asthma is an inflammatory airway disease that often starts in childhood and is reversible with medication.
- COPD is a progressive loss of lung function, usually linked to long‑term smoking or exposure to pollutants.
- Symptoms overlap (cough, wheeze, shortness of breath) but triggers and long‑term outlook differ.
- Spirometry is the primary test that separates the two by measuring reversibility.
- Treatment for asthma focuses on controlling inflammation, while COPD management centers on bronchodilation and lifestyle changes.
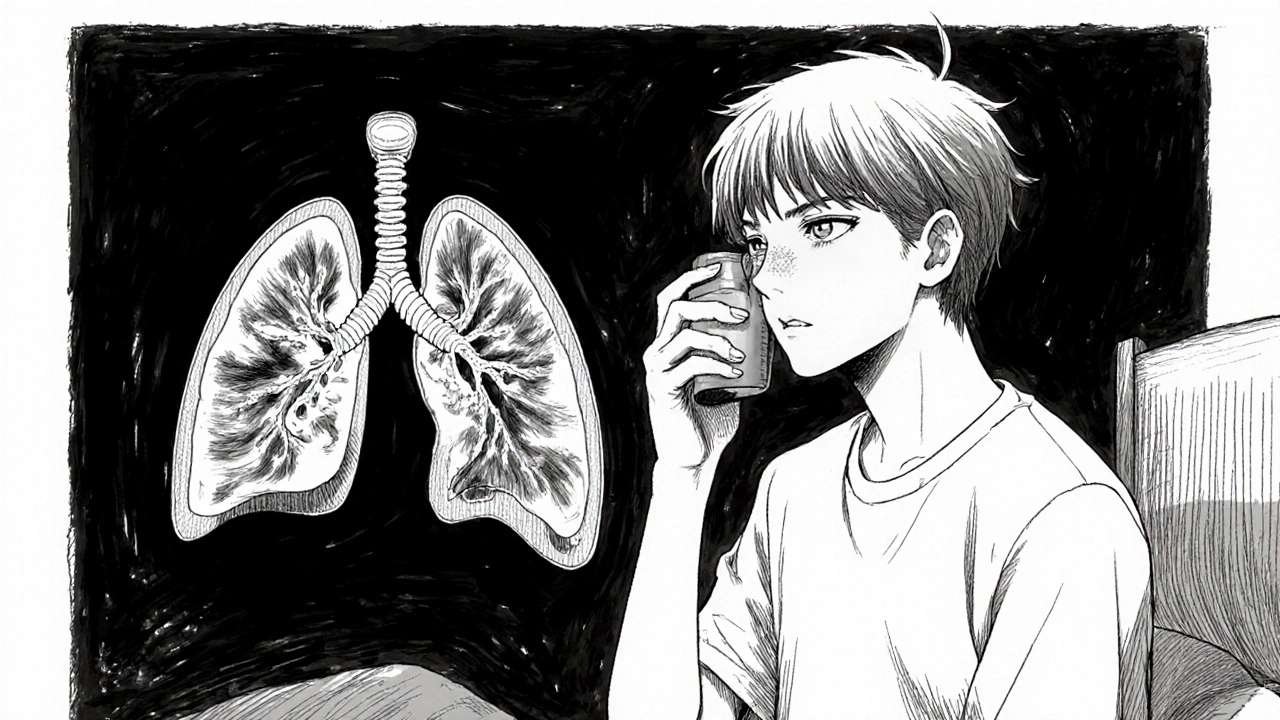
What Is Bronchial Asthma?
Bronchial Asthma is a chronic inflammatory disease of the airways that leads to periodic narrowing, mucus production, and heightened sensitivity to triggers. The inflammation is driven by a combination of genetic predisposition and environmental factors like allergens, viral infections, or exercise. When exposed, the airway muscles tighten (bronchoconstriction) and the lining swells, causing the classic wheeze and shortness of breath.
Because the airway changes are largely reversible-often after a puff of a rescue inhaler-most people can experience symptom‑free periods between attacks. Asthma can start at any age, but many cases appear in childhood and persist into adulthood.
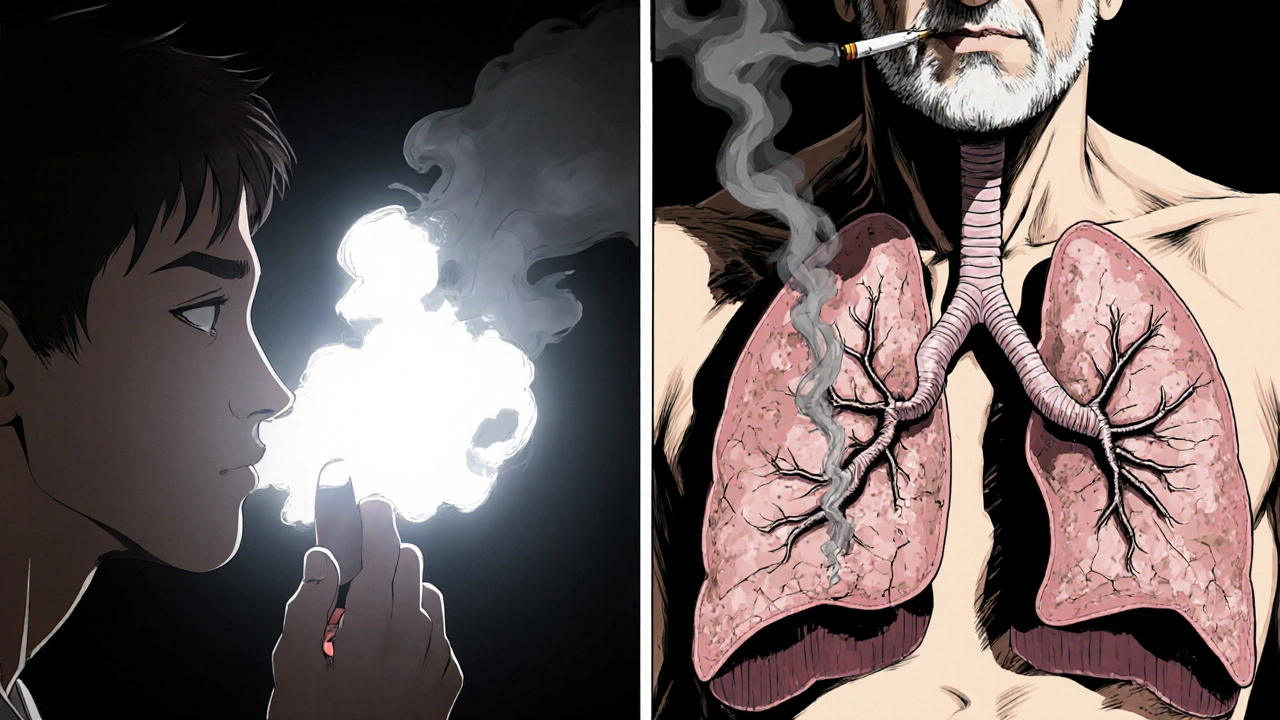
What Is Chronic Obstructive Pulmonary Disease (COPD)?
Chronic Obstructive Pulmonary Disease (COPD) is a progressive lung disorder characterized by irreversibly reduced airflow. The disease bundles two main pathologic components: Emphysema, which destroys alveolar walls, and Chronic Bronchitis, which causes persistent cough and mucus overproduction. COPD is strongly linked to long‑term exposure to noxious particles-most commonly cigarette smoke, but also air pollution or occupational dust.
Unlike asthma, the airway obstruction in COPD is only partially reversible, and lung function continues to decline over time, making early detection crucial.
Core Differences at a Glance
| Aspect | Bronchial Asthma | COPD |
|---|---|---|
| Typical Onset | Childhood‑to‑early adulthood | Usually after 40 years, often with smoking history |
| Primary Cause | Allergen or irritant‑induced airway inflammation | Long‑term exposure to smoke or pollutants |
| Reversibility | Marked reversibility with bronchodilators | Limited reversibility; airflow obstruction persists |
| Key Pathophysiology | Airway inflammation, eosinophilic infiltrates | Emphysema + chronic bronchitis, loss of elastic recoil |
| Diagnostic Test | Spirometry showing >12% improvement post‑bronchodilator | Spirometry with Spirometry showing < 70% predicted FEV1, minimal reversibility |
| Typical Symptoms | Wheeze, episodic cough, night‑time symptoms | Persistent cough, sputum production, dyspnea on exertion |
| First‑line Treatment | Inhaled Corticosteroids + as‑needed Bronchodilators | Long‑acting Bronchodilators (LABA/LAMA) and smoking cessation |
| Long‑term Outlook | Good control possible; many live symptom‑free | Progressive decline; management focuses on slowing loss |
Symptoms: What Overlaps and What Doesn’t
Both diseases can present with a cough, wheezing, and shortness of breath. However, the pattern matters. Asthma often worsens at night or early morning and spikes after exposure to specific triggers-pollen, pet dander, cold air, or exercise. COPD’s cough is usually productive (producing mucus) and persists throughout the day, especially in the mornings.
If you’ve noticed that a quick‑acting inhaler relieves the breathlessness almost completely, you’re likely dealing with asthma. On the other hand, if the breathlessness remains despite bronchodilators, COPD is more probable.
Triggers vs. Risk Factors
Asthma’s hallmark is hyper‑responsiveness to triggers: allergens, viral infections, strong odors, or even stress. This hyper‑responsiveness is linked to an overactive immune response that involves Airway Inflammation and eosinophils.
COPD’s risk factors are cumulative irritants. Smoking remains the number‑one culprit, accounting for roughly 85% of cases worldwide. Occupational dusts (mining, construction) and chronic exposure to indoor air pollutants also play roles.
Diagnostic Tools: Spirometry and Beyond
Both conditions rely heavily on Spirometry, a simple breathing test that measures Forced Expiratory Volume in one second (FEV1) and Forced Vital Capacity (FVC). The key differentiator is reversibility:
- Baseline spirometry is performed.
- Patient inhales a short‑acting bronchodilator.
- Repeat spirometry after 15 minutes.
A rise of ≥12% and 200 mL in FEV1 indicates asthma. Minimal change points toward COPD. In ambiguous cases, doctors may order a Pulmonary Function Test that includes diffusion capacity (DLCO) to assess emphysema severity.
Management Strategies
While both diseases use inhalers, the goals differ.
Asthma Management
- Control medication: Regular Inhaled Corticosteroids to dampen inflammation.
- Rescue inhaler (short‑acting Bronchodilator) for acute symptoms.
- Trigger avoidance: dust‑mite covers, air purifiers, flu vaccine.
- Action plan: written steps for worsening symptoms.
COPD Management
- Smoking cessation-most impactful intervention.
- Long‑acting bronchodilators (LABA/LAMA) to keep airways open.
- Pulmonary rehabilitation: exercise, breathing techniques.
- Vaccinations (influenza, pneumococcal) to prevent infections.
- Oxygen therapy for advanced disease.
When Asthma and COPD Co‑exist
It’s possible for a patient to have both-often called Asthma‑COPD Overlap Syndrome (ACOS). These individuals exhibit features of reversible airway obstruction (asthma) plus the chronic decline of COPD. Management blends both approaches: inhaled corticosteroids for the asthma component and long‑acting bronchodilators for COPD.

When to Seek Medical Attention
- Sudden, severe breathlessness that doesn’t improve with a rescue inhaler.
- Persistent cough with colored sputum, fever, or chest pain.
- Increasing frequency of nighttime symptoms.
- Any new wheeze after a period of stability.
Early evaluation can differentiate the two conditions, allowing tailored treatment and preventing complications like asthma attacks or COPD exacerbations.
Quick Checklist for Self‑Assessment
- Do you notice symptoms mainly after exposure to allergens or exercise? → Likely asthma.
- Is your cough productive and worse in the mornings? → Consider COPD.
- Do you respond dramatically to a short‑acting inhaler? → Points to asthma.
- Do you have a long history of smoking or occupational dust exposure? → Suggests COPD.
Frequently Asked Questions
Can asthma turn into COPD?
Asthma itself doesn’t cause COPD, but long‑term smoking in an asthmatic can lead to COPD. The two diseases have separate pathways, though overlap can occur.
Is there a cure for either condition?
Asthma can often be well‑controlled, letting people live symptom‑free. COPD is progressive; treatment focuses on slowing decline, not curing.
Do I need separate inhalers for asthma and COPD?
If you have both, doctors usually prescribe a combination inhaler that includes a corticosteroid (for asthma) and a long‑acting bronchodilator (for COPD). Individual needs can vary.
How often should I get spirometry tests?
For stable asthma, once a year is typical. COPD patients often need testing every 6‑12 months to track progression.
Can lifestyle changes improve my condition?
Absolutely. Asthma benefits from allergen control, regular exercise, and weight management. COPD improvement hinges on quitting smoking, staying active, and good nutrition.
Next Steps
If you suspect you have either condition, schedule a lung function test with a primary‑care provider or pulmonologist. Bring a list of your symptoms, any triggers you’ve noticed, and a smoking history if applicable. Accurate diagnosis opens the door to personalized treatment-and better quality of life.
Understanding the nuances between bronchial asthma and COPD empowers you to ask the right questions, follow the correct medication plan, and avoid unnecessary panic when breathlessness strikes.
Michaela Dixon
October 23, 2025 AT 17:23Reading this guide feels like opening a map that finally shows where the fog of breathlessness lifts. It walks you through the tangled forest of asthma and COPD with a lantern of plain language. You discover that asthma is often a childhood companion that can be tamed with a well‑timed puff of medicine. COPD, on the other hand, sneaks in later like a stubborn weed that refuses to wilt even when you pull at it. The author points out that spirometry is the magic wand that separates the two by measuring how much the lungs can bounce back after a bronchodilator. When the numbers jump more than a dozen percent you are likely looking at asthma. If they stay stubbornly low you are staring at COPD. The table in the middle of the article acts like a side‑by‑side comparison that a coach would use to train a mixed‑skill team. It lists onset age smoking history reversibility and the typical daily symptoms in bright columns. You also learn that asthma’s inflammation can be calmed with inhaled steroids while COPD relies on bronchodilators and lifestyle changes. The guide reminds you that quitting smoking is the single most powerful move for COPD patients and a wise choice for anyone with breathing trouble. It even mentions the overlap syndrome where the two diseases dance together and you need a hybrid treatment plan. The section on triggers paints a vivid picture of pollen, dust, cold air and stress kicking asthma into overdrive. Meanwhile the smog and cigarette smoke are described as the slow poison that erodes lung tissue in COPD. The author does not shy away from the sobering fact that COPD is progressive and cannot be cured but can be slowed. Yet the tone stays hopeful by urging regular check‑ups and pulmonary rehab to keep the lungs as strong as possible. Finally the checklist at the end serves as a quick self‑assessment tool that anyone can use before booking an appointment. In sum the article is a compass that points you toward the right diagnosis and the right next steps for a clearer breath.
Dan Danuts
October 31, 2025 AT 18:50Great breakdown! I love how you laid out the differences in a way that even my grandma could get. This will definitely help people take the right steps and not get stuck in confusion. Keep the good stuff coming!
Dante Russello
November 8, 2025 AT 21:17Thanks for sharing this detailed guide, it really hits the nail on the head, especially when it comes to emphasizing spirometry as the key diagnostic tool, which many people overlook, and the clear table comparison makes it easy to see the distinctions, plus the practical advice on lifestyle changes, like quitting smoking, is spot on, and the mention of overlap syndrome adds depth, reminding us that respiratory health isn’t always black and white, and the checklist at the end is a handy quick reference, I’ll definitely pass this on to friends who are dealing with breath issues, great job!
James Gray
November 16, 2025 AT 23:43Yo Dan great point man i totally feel u the vibe s super motivating keep it up bro
Scott Ring
November 25, 2025 AT 02:10I hear you all, and I think the biggest takeaway is that knowing the difference can actually reduce anxiety. When you know which meds work best and why, you feel more in control of your health.
Shubhi Sahni
December 3, 2025 AT 04:37Absolutely, Scott, you’ve nailed it, especially the part about regular check‑ups, which are crucial, and the emphasis on quitting smoking, which can dramatically improve outcomes, plus the reminder about vaccines, which many people forget, really rounds out a comprehensive approach.
Danielle St. Marie
December 11, 2025 AT 07:03This is exactly why 🇺🇸 leads in medical education 😂
keerthi yeligay
December 19, 2025 AT 09:30Very helpful guide. Good job.