Anaphylaxis: Recognizing the Signs and Why Epinephrine Saves Lives
 Dec, 24 2025
Dec, 24 2025
One minute you’re eating a peanut butter sandwich. The next, your throat feels tight, your skin breaks out in hives, and you can’t catch your breath. This isn’t just a bad reaction-it’s anaphylaxis, a life-threatening allergic emergency that can kill in minutes if not treated right away. There’s no time to wait, no time to call around, no time to hope it gets better. The only thing that stops it? Epinephrine.
What Exactly Is Anaphylaxis?
Anaphylaxis isn’t a rash or a stomachache. It’s your immune system going into overdrive, releasing chemicals that crash your blood pressure, swell your airways, and shut down your body’s ability to breathe or circulate blood. It doesn’t come slowly. It hits fast-often within seconds or minutes after exposure to an allergen. You might feel a tingling in your mouth, then your lips puff up, your voice gets hoarse, and your chest feels like it’s being squeezed. Some people vomit or feel dizzy. Others just feel like something is terribly wrong. According to the Resuscitation Council UK’s 2021 guidelines, anaphylaxis is diagnosed when you have sudden symptoms involving your skin (like hives or swelling), plus one or more of these: trouble breathing, low blood pressure, or ongoing stomach pain. And here’s the key: you don’t need all the symptoms. If you’ve been exposed to something you’re allergic to and you’re having any serious reaction, treat it as anaphylaxis-right away. Common triggers? Foods like peanuts, tree nuts, shellfish, and eggs. Insect stings from bees or wasps. Medications, especially penicillin. Latex. For kids, food is the biggest culprit. For adults, it’s often stings or drugs. And it’s not rare. About 1.6% of Americans-over 5 million people-have had anaphylaxis at least once. The numbers are rising, especially with peanut allergies in children tripling since the 1990s.Why Epinephrine Is the Only Thing That Works
You’ve probably heard people say, “Just take an antihistamine.” That’s dangerous advice. Antihistamines like Benadryl do nothing to stop the collapse of your airway or your blood pressure. A Cochrane review from 2012 found they have zero effect as a standalone treatment for anaphylaxis. Corticosteroids? They might help prevent a second wave of symptoms hours later, but they won’t save you in the moment. Epinephrine is the only treatment that directly reverses the life-threatening changes. It tightens blood vessels to raise your pressure, opens your airways so you can breathe, and stops the runaway immune response. It works in minutes. Studies show 85% of patients improve within five minutes if epinephrine is given early. If you wait longer than 15 minutes? Your chance of dying goes up dramatically. The science is clear: 97% of emergency doctors agree epinephrine is the only first-line treatment. Dr. Robert Wood from Johns Hopkins says it bluntly: “There is no substitute.” Delaying it is the single biggest reason people die from anaphylaxis.How to Use an Epinephrine Auto-Injector
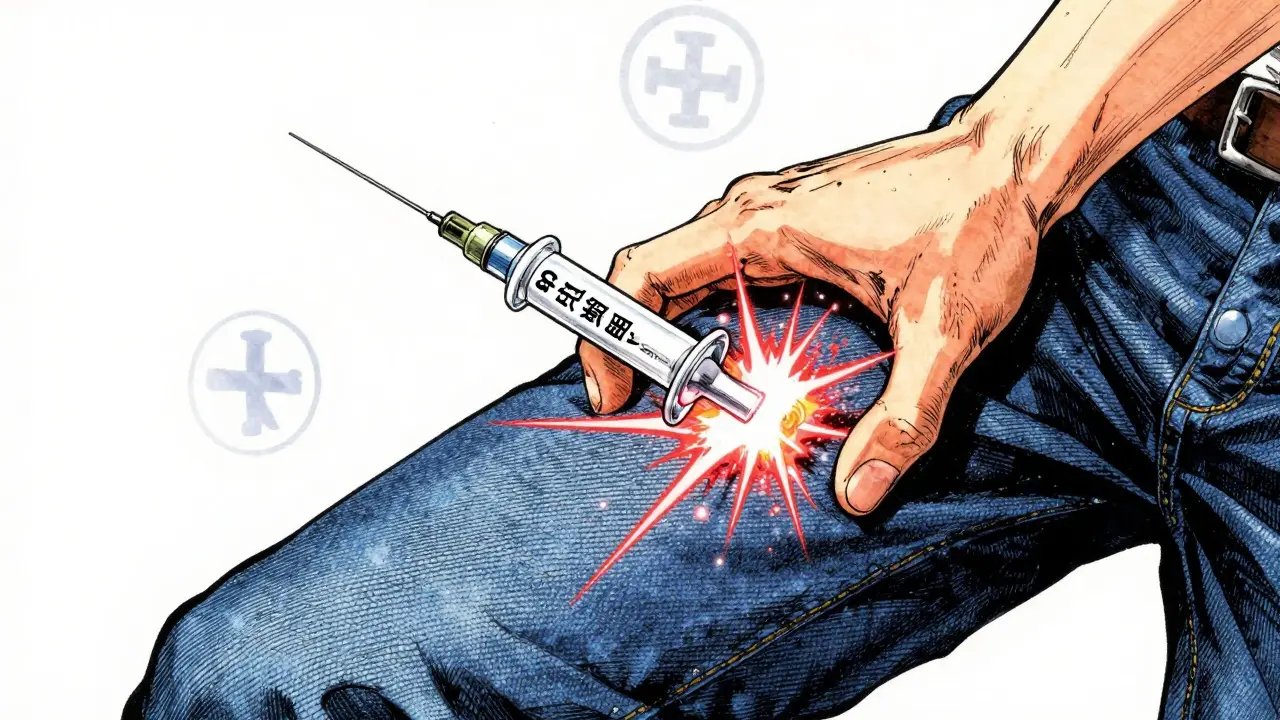
Epinephrine comes in auto-injectors-small, pen-like devices you carry with you. The most common brands are EpiPen, Auvi-Q, and Adrenaclick. They’re not complicated, but you have to know how to use them. Here’s the simple steps:- Remove the safety cap.
- Place the tip against the outer thigh-through clothing if needed.
- Push hard until you hear a click.
- Hold it in place for 3 seconds.
- Remove and massage the area for 10 seconds.
What Happens After the Injection?
Even if you feel better after the shot, you still need to call 911 or go to the ER. Anaphylaxis can come back-sometimes hours later. This is called a biphasic reaction. About 20% of people experience it. That’s why guidelines now say high-risk patients need to be observed for at least 12 hours. You also need to be monitored for heart rhythm changes. Epinephrine can cause a fast heartbeat or palpitations, but that’s a sign it’s working. Don’t panic. The ER team will check your vitals, give oxygen if needed, and make sure you’re stable. And here’s something no one talks about enough: you need a written action plan. Only 37% of people discharged after an anaphylaxis episode get one. That’s unacceptable. Your plan should include your triggers, how to use your injector, when to call for help, and who to contact. Keep a copy at home, at work, and give one to your school or caregiver.Why People Don’t Use It-And How to Fix It
You’d think everyone with a prescription would carry their injector. But they don’t. A survey by the Asthma and Allergy Foundation found only 65% of people carry theirs consistently. Why? - They don’t recognize the symptoms. 58% of adults can’t tell the difference between a mild reaction and anaphylaxis. - They’re scared of the needle. One in five patients avoid using it because of needle phobia. - They wait too long. 43% delay because they think, “Maybe it’s not that bad.” - They forget to check the expiration date. Devices expire in 12-18 months. Epinephrine loses potency over time. The fix? Practice. Use a training device every month. Many pharmacies give them for free. Teach your kids, your partner, your coworkers. Put a reminder on your phone. Store your injector at room temperature-don’t leave it in the car or in the sun. Heat ruins it. And if cost is an issue? Generic versions now make up 70% of prescriptions in the U.S. Out-of-pocket costs have dropped from $325 in 2016 to $185 today. Some insurance plans cover them fully. Ask your pharmacist. Don’t skip this because you think it’s too expensive. It’s not. It’s lifesaving.
New Options and What’s Coming
In August 2023, the FDA approved Neffy-a nasal spray version of epinephrine. No needle. Just spray one dose into each nostril. It’s a game-changer for people who can’t tolerate injections. Early data shows it works as fast as the injection. Other innovations are coming. Smart injectors with Bluetooth that alert your emergency contacts when used. Longer-lasting formulas in development. And school programs are expanding: all 50 U.S. states now require stock epinephrine in schools, and 34 states will mandate training for staff by 2025. But none of this replaces the need for immediate action. The most important tool is still the auto-injector in your pocket. The most important skill is knowing when to use it.Final Warning: Don’t Wait
Anaphylaxis doesn’t care if you’re busy, tired, or unsure. It doesn’t wait for a doctor. It doesn’t care if you think it’s “just a little swelling.” If you’re exposed to your known allergen and something feels wrong-act. Inject. Call 911. Even if you’re wrong, you’re safe. If you wait, you might not get another chance. Epinephrine isn’t perfect. It’s expensive. It expires. It can be scary. But it’s the only thing that works. And when seconds count, you don’t need the best option-you need the one that saves lives. That’s epinephrine.Can antihistamines like Benadryl treat anaphylaxis?
No. Antihistamines do not stop airway swelling, low blood pressure, or respiratory failure-the main dangers of anaphylaxis. They may help with mild itching or hives, but they have zero effect as a standalone treatment. Delaying epinephrine to take an antihistamine can be deadly.
Where should I inject epinephrine?
Always inject into the outer thigh-the vastus lateralis muscle. This area has the fastest absorption. You can inject through clothing if needed. Never inject into the buttocks, arm, or hand. These areas absorb the drug too slowly, delaying life-saving effects.
Can I reuse an epinephrine auto-injector?
No. Auto-injectors are single-use devices. Even if you think you didn’t fully activate it, don’t try to reuse it. The needle may be damaged, or the dose may be incomplete. Always use a new one. Keep two on hand at all times in case a second dose is needed.
Do I need to go to the hospital after using epinephrine?
Yes. Even if you feel fine after the injection, you must go to the ER. Anaphylaxis can return hours later in what’s called a biphasic reaction. You need monitoring for at least 4-12 hours, depending on your risk factors. Never assume one shot means you’re out of danger.
How often should I check my epinephrine’s expiration date?
Check every month. Most auto-injectors expire in 12 to 18 months. Epinephrine loses potency over time, especially if exposed to heat or light. Set a calendar reminder. Replace it before it expires. Never use an expired injector unless it’s a true emergency and no other option exists.
Is there a needle-free option for epinephrine?
Yes. Neffy, a nasal spray approved by the FDA in August 2023, delivers epinephrine without a needle. It’s just as fast and effective as the injection for most people. It’s a great alternative for those with needle phobia or difficulty with injections, but it’s not yet widely available everywhere. Ask your allergist if it’s right for you.
Knowing the signs and acting fast can save your life-or someone else’s. Keep your injector accessible. Train your family. Don’t wait for perfect conditions. Anaphylaxis doesn’t wait. Neither should you.
Mussin Machhour
December 24, 2025 AT 16:26Just carried my EpiPen to the grocery store yesterday. Felt weird at first-like I was being paranoid. Then I saw a kid with a peanut butter sandwich next to my cart. My hand went straight to my pocket. Better safe than sorry. This stuff saves lives, period.
Katherine Blumhardt
December 26, 2025 AT 02:57i got an epipen last year after my cousin almost died at a birthday party 😭 no one knew what was happening until someone yelled ‘IS HE ALLERGIC TO PEANUTS’ and i pulled mine out and used it on him. he’s fine now. but like… why do people still think benadryl works???
Christopher King
December 26, 2025 AT 13:17Let me tell you something the medical-industrial complex doesn’t want you to know. Epinephrine isn’t the miracle cure-it’s the *controlled release* of a synthetic adrenaline surge designed to force your body into survival mode while the system scrambles to bill you $600 for a 5-minute ER visit. They keep you scared. They keep you buying. They keep you dependent. But here’s the real truth: your body *can* heal itself if you stop treating it like a broken machine. Epinephrine? It’s a bandage on a bullet wound.
Linda B.
December 28, 2025 AT 11:43So let me get this straight… the government pushes epinephrine because it’s profitable… but they also approve nasal sprays now? Coincidence? Or is this just another way to upsell us new devices every 18 months while the real solution-avoiding allergens altogether-is buried under corporate lobbying? I’ve seen the documents. They’re not hiding it. They’re just making it harder to read.
Bailey Adkison
December 30, 2025 AT 11:39Correction: The Cochrane review didn’t say antihistamines have ‘zero effect.’ It said they have no effect on mortality or airway compromise. Hives? Maybe. Breathing? No. You’re misrepresenting the data. Also, ‘epinephrine’ is the correct term. ‘Adrenaline’ is outdated. Fix your language before you preach.
Ben Harris
December 31, 2025 AT 22:05My sister’s a nurse. She told me once she saw a guy die because his epinephrine was expired. He had it in his glove compartment. In Arizona. In July. He thought ‘it’s just one day past’ and then he was gone. I carry two now. One in my bag. One taped to my phone case. I don’t care how weird it looks. I’d rather be the guy who looks like a nutjob than the guy who’s a statistic.
Gary Hartung
January 1, 2026 AT 11:44Oh, so now we’re supposed to carry a pen-shaped death device in our pockets like it’s a fancy lip balm? And pray it doesn’t explode in the sun? And then, when we finally use it, we’re supposed to traipse down to the ER like obedient little patients while the hospital staff quietly chuckle about the ‘anaphylaxis revenue stream’? This isn’t medicine. It’s performance art with a price tag. I’d rather die quietly than be part of this circus.
Zabihullah Saleh
January 2, 2026 AT 07:15There’s something deeply human about this. We live in a world where we’re told to fear everything-food, chemicals, needles-and yet the one thing that can save us is the very thing we’re taught to avoid. Epinephrine isn’t just chemistry. It’s trust. Trust in your body’s warning. Trust in your own courage. Trust that someone, somewhere, cared enough to make this tool exist. And now we’re supposed to carry it like a secret weapon. Maybe that’s the real lesson here: we’re not helpless. We just forgot how brave we can be.
Lindsay Hensel
January 3, 2026 AT 15:48My daughter has a peanut allergy. We’ve had two near-misses. I carry two injectors. I taught her to use them at age six. I don’t care if it’s ‘dramatic.’ I care that she’s alive. If you’re not prepared, you’re gambling with her life. And that’s not bravery. That’s negligence.