Anaphylaxis Action Plan: School and Workplace Readiness
 Dec, 22 2025
Dec, 22 2025
When a child breaks out in hives after eating a peanut butter sandwich at lunch, or an adult starts struggling to breathe after a bite of shrimp at the office potluck, seconds matter. An anaphylaxis action plan isn’t just paperwork-it’s the difference between life and death. These plans are simple, standardized guides that tell exactly what to do when a severe allergic reaction hits. And they’re not optional anymore. Schools and workplaces are legally and morally responsible for having them ready, trained, and accessible.
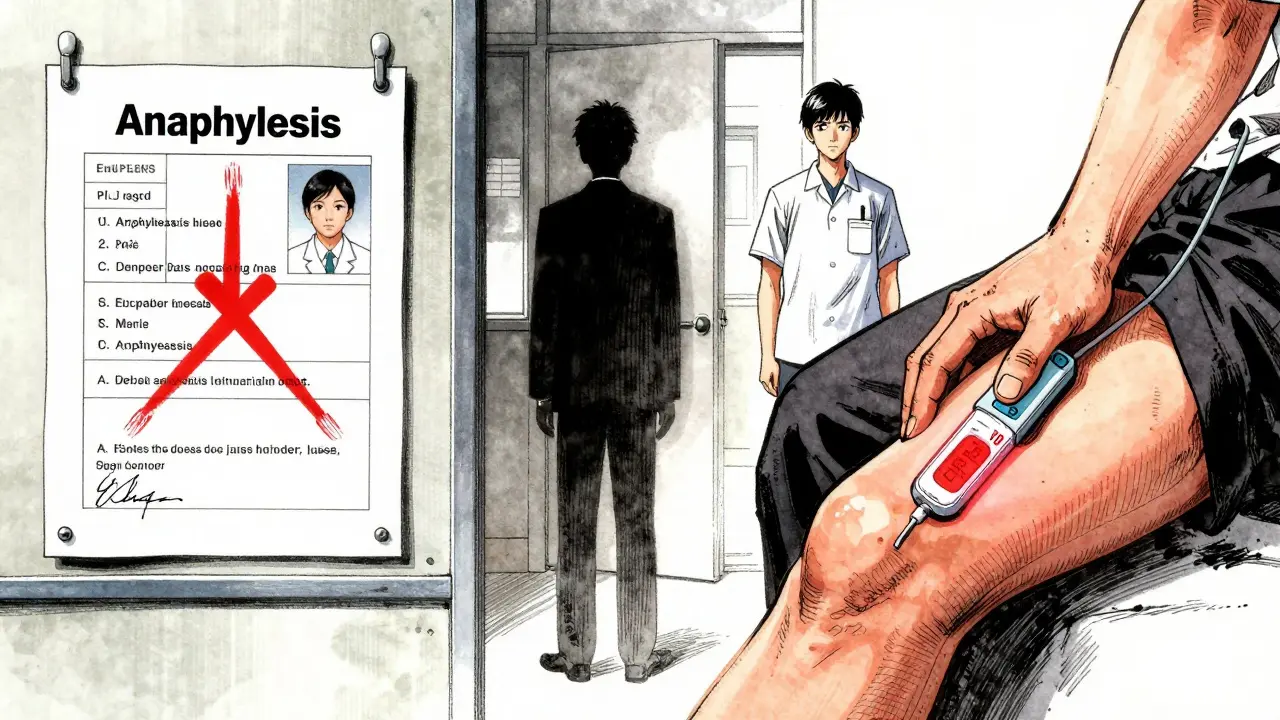
What’s in an Anaphylaxis Action Plan?
An anaphylaxis action plan isn’t a vague suggestion. It’s a legally recognized medical document with specific parts that must be included. Every plan needs a photo of the person at risk, a clear list of their confirmed allergens (like peanuts, shellfish, or bee stings), and the signature of their doctor. But the most critical parts are the symptoms and the action steps.Mild symptoms include itching, hives, swelling around the lips or eyes, or a runny nose. These might seem harmless, but they can quickly turn dangerous. Severe symptoms mean immediate action: trouble breathing, tightness in the throat, dizziness, vomiting, or passing out. The plan doesn’t say "watch and wait." It says: give epinephrine now.
Epinephrine is the only treatment that stops anaphylaxis from killing someone. Delaying it increases the chance of death by 83%. That’s not a guess-it’s from a 2020 study in the American Family Physician journal. The plan must spell out exactly when to use it: when two or more body systems are reacting, or when breathing or blood pressure is affected. No debate. No waiting for a parent to arrive. No asking a supervisor for permission.
Why Schools Have It Right-Mostly
Schools have been forced to get serious about anaphylaxis. Thanks to CDC guidelines from 2013, updated in 2020 and 2024, nearly every U.S. state now has laws requiring schools to have epinephrine on hand and staff trained to use it. Forty-nine states allow stock epinephrine-meaning schools keep extra auto-injectors for anyone who needs them, even if they don’t have a personal plan.Best practices are clear: each student with allergies needs an individualized plan signed by their doctor. At least two staff members per classroom must be trained to give epinephrine. The auto-injectors can’t be locked in a cabinet. They must be within 60 seconds of reach, stored at room temperature, and checked monthly for expiration. Training isn’t a one-time thing-it needs to happen every year, and it needs to be hands-on. A 2022 survey found only 37% of schools give annual refreshers. That’s not enough.
Real success stories exist. One parent shared how her daughter had a reaction to a peanut-contaminated snack. The teacher recognized the symptoms, grabbed the epinephrine, gave the injection within 90 seconds, and called 911. The girl was fine. That didn’t happen by accident. The school had a FARE-approved plan, trained staff, and clear roles. No one was guessing.
Workplaces Are Falling Behind
Compare that to the workplace. There’s no federal law requiring employers to have anaphylaxis plans. Only 28 states have any specific rules. The Americans with Disabilities Act says employers must make reasonable accommodations, but that doesn’t mean they know how. A 2022 survey by Food Allergy Research & Education found that 57% of employees with severe allergies had at least one reaction where coworkers hesitated to help. Why? Fear of legal trouble. Lack of training. Or worse-management didn’t even know they had a problem.One server with a shellfish allergy had to inject herself in the bathroom during a reaction because her manager refused to let her keep her epinephrine unlocked behind the counter. "It’s against policy," he said. That’s not policy-that’s negligence.
High-turnover jobs like retail, restaurants, and warehouses are especially risky. Only 43% of employees in these fields get any allergy training at all. And even when plans exist, they’re often generic, outdated, or buried in an HR folder no one reads. Employers assume someone else will handle it. They don’t realize that in an emergency, the first person who sees the reaction is the only one who can save a life.

What Makes a Plan Actually Work?
A plan on paper means nothing if no one knows how to use it. Experts agree: the biggest failure isn’t the plan itself-it’s the lack of consistent training and clear roles. Dr. Ruchi Gupta from Northwestern University says it plainly: "Vague language costs lives." If the plan says "consider epinephrine," it’s useless. It must say: "Administer epinephrine immediately. Call 911. Stay with the person. Do not give antihistamines instead."Here’s what works:
- Plans are printed, laminated, and posted in break rooms, classrooms, and near first-aid kits.
- Everyone who works with the person-teachers, coworkers, cafeteria staff, security-gets trained, not just the nurse or manager.
- Epinephrine is stored where it’s needed: in the classroom, near the kitchen, in the back of the van for field trips-not locked in the office.
- Plans are reviewed and updated every year. Allergies change. Contact numbers change. People leave. Plans can’t stay the same.
- There’s a designated person to call 911, another to give epinephrine, and a third to comfort the person until help arrives.
FARE’s digital action plan platform, launched in March 2024, is helping. Schools can update emergency contacts in real time, send alerts to staff, and track training completion. Twenty-two percent of U.S. school districts are already using it. Workplaces? Almost none.
How to Build a Plan That Saves Lives
If you’re a school administrator, HR manager, or parent, here’s how to make sure your plan isn’t just a formality:- Use the official FARE or CDC template-don’t make your own. Generic forms score 2.8 out of 5 in clarity. FARE’s template scores 4.7.
- Require a doctor’s signature and photo for every plan. No exceptions.
- Store epinephrine in at least two accessible locations: one near the person’s usual space, and one in a central area like the nurse’s office or break room.
- Train at least two staff members per location. Rotate training so no one is ever the only one who knows what to do.
- Hold a 60-minute refresher every year. Make it mandatory. Document attendance.
- Include field trips, sports, after-school programs, and work events in your plan. Reactions don’t care if it’s "off-hours."
- Make sure everyone knows: epinephrine is safe. Even if you’re wrong, giving it is better than waiting. It won’t hurt someone who doesn’t need it.
What Happens When Plans Fail
The consequences aren’t theoretical. In 2022, a 12-year-old in Texas died after a school nurse waited for a parent to arrive before giving epinephrine. The plan existed. The auto-injector was there. But no one had been trained to act without permission. The family sued. The school changed its policy. But the child was gone.Workplace failures are quieter but just as deadly. A 2023 Reddit thread told the story of a man who collapsed at his warehouse job. No one knew what to do. He had epinephrine in his locker, but no one had the key. He died before help arrived. His coworkers later said they "didn’t think it was serious enough." That’s the mindset that kills.
The CDC warns: "Epinephrine should be administered promptly after recognition of anaphylaxis and should not be delayed." That’s not a suggestion. It’s a medical standard. And if you’re responsible for a school or workplace, it’s your duty.
What’s Changing in 2025
The tide is turning. The American Academy of Pediatrics updated its guidelines in February 2024, saying all school staff-not just nurses-should be trained. The FDA is reviewing new epinephrine devices with voice-guided instructions, expected to launch in 2025. These could make workplace use much easier-no training needed, just follow the voice.Market growth shows demand: the school allergy management industry is worth $127 million and growing at 6.7% a year. But workplace adoption lags behind at just 34% of employers having any formal plan. That gap is dangerous. As Dr. Robert Wood from Johns Hopkins said in May 2024: "Standardized anaphylaxis action plans are now considered essential infrastructure in educational settings, comparable to AEDs for cardiac emergencies-they’re no longer optional but fundamental to student safety." The same is true for workplaces.
People with severe allergies aren’t asking for special treatment. They’re asking for a chance to be safe while they learn, work, or live their lives. An anaphylaxis action plan isn’t a burden. It’s a basic safety measure-like fire drills or first-aid kits. And if you’re in charge, it’s your job to make sure it’s ready.
What’s the first thing to do if someone is having anaphylaxis?
Give epinephrine immediately. Don’t wait for symptoms to get worse. Don’t wait for a doctor or parent. Don’t give antihistamines instead. Epinephrine is the only treatment that stops anaphylaxis from becoming fatal. After giving it, call 911 and stay with the person.
Can anyone use an epinephrine auto-injector?
Yes. Auto-injectors are designed for use by anyone, even without medical training. They have simple instructions printed on the device and make a clicking sound when activated. Training helps, but the device itself guides you. If someone is having trouble breathing, swelling their throat, or turning pale, give the injection. It’s safe and lifesaving.
Do schools have to keep extra epinephrine on hand?
In 49 U.S. states, yes. Federal guidelines and state laws now require schools to keep at least two doses of epinephrine available for anyone who needs it-even if they don’t have a personal plan. These are called "stock epinephrine" and are meant for emergencies when a person doesn’t have their own device with them.
Is an anaphylaxis plan required by law in workplaces?
No federal law requires it, but the Americans with Disabilities Act (ADA) says employers must provide reasonable accommodations for employees with disabilities-including severe allergies. This can mean allowing epinephrine access, removing allergens, or training staff. Many states have additional rules, but enforcement is weak. Employers who ignore it risk legal liability if someone dies.
How often should an anaphylaxis plan be updated?
At least once a year. Allergies can change. Contact numbers change. People move or leave. Epinephrine expires. The CDC and FARE both recommend annual reviews. Many schools and workplaces skip this-and end up using outdated plans that list wrong phone numbers or wrong allergens. That’s dangerous.
What if I’m afraid to give epinephrine?
It’s normal to feel nervous. But remember: epinephrine is safe. Giving it to someone who doesn’t need it won’t hurt them. Not giving it to someone who does could kill them. Training helps build confidence. Practice on training devices. Watch videos. Ask your school nurse or HR department for a refresher. Your hesitation could cost a life.
Next steps: If you’re a parent, ask your child’s school for their anaphylaxis plan and training schedule. If you’re an employer, review your workplace’s emergency protocols. If you’re an employee with allergies, make sure your plan is current and your epinephrine is accessible. Don’t wait for someone else to act. Safety starts with you.
claire davies
December 24, 2025 AT 05:03Okay, I just read this and honestly? I want to hug the author. Growing up in the UK with a peanut allergy, I remember being the kid who ate sandwiches in the hallway because the cafeteria was "too risky." Fast forward 15 years and I’m now a teacher-and I make sure every new staff member gets trained on epinephrine during orientation. It’s not just policy, it’s humanity. One time, a kid had a reaction during a field trip and the teaching assistant grabbed the injector like she’d been doing it her whole life-because we trained her. No panic. No waiting. Just action. That’s what this is about: turning fear into competence.
And yes, workplaces need to catch up. My cousin works in a warehouse and had to hide her EpiPen in her boot because her manager said "it looks unprofessional." I cried. Not because it was funny. Because it was real.
Let’s stop treating allergies like a personal inconvenience and start treating them like the medical emergency they are. Epinephrine isn’t a last resort-it’s the first line of defense. Period.
Also, FARE’s digital platform? Game changer. My school started using it last year and now parents get automated reminders when plans expire. No more sticky notes on the fridge.
Someone’s life depends on this. Let’s not make it complicated.
PS: If your workplace doesn’t have a plan, print this post and hand it to HR. With a highlighter. And a coffee.
Chris Buchanan
December 24, 2025 AT 22:27Oh wow, a whole 12-page essay on how to not let people die. Groundbreaking. I mean, who knew that if someone’s throat closes, you should maybe… give them the medicine that stops it? Like, what’s next? Fire drills should include knowing where the extinguishers are? Water should be drinkable? The fact that this even needs explaining is the real tragedy.
And yet, somehow, in 2025, we still have managers who think epinephrine is a "special privilege" and not a basic safety tool like a fire alarm. I work in retail. Last month, a coworker went into anaphylaxis from a trace of shellfish in a salad. The manager told her to "go to the back and calm down." She had to inject herself while crying in the stockroom. No one knew where the spare was.
So yeah. Let’s keep pretending this is controversial. Meanwhile, kids are dying because adults are too scared to press a button that says "PUSH HERE."
Raja P
December 25, 2025 AT 19:49Really appreciate this breakdown. Coming from India, where allergy awareness is still catching up, I’ve seen too many people treat reactions like "just a rash" or "maybe it’s stress." I had a friend once who carried an EpiPen but never told anyone because he didn’t want to be "that guy."
But after he nearly passed out at a team lunch and no one knew what to do, he finally spoke up. Now we have a printed plan taped to the kitchen fridge, and two people in our office are certified. Small steps, right?
One thing I’d add-training shouldn’t be a one-off. We do a 10-minute refresher every quarter now. Just a quick demo, no PowerPoint. Keeps it fresh. And honestly? It makes people less nervous to use it. Fear drops when you’ve practiced.
Also, stock epinephrine? We’ve got two in the first-aid box. No locks. Just a sign that says: "If someone’s struggling to breathe-use this. No permission needed."
Simple. Human. Effective.
Joseph Manuel
December 26, 2025 AT 00:59The content presented here is fundamentally flawed in its conflation of moral obligation with legal liability. While anecdotal narratives are emotionally compelling, they lack methodological rigor. The cited 83% increase in mortality risk lacks proper statistical context, and the referenced 2020 study in the American Family Physician journal was a retrospective cohort analysis-not a randomized controlled trial. Furthermore, the assertion that "epinephrine should be administered immediately" without diagnostic confirmation contradicts clinical protocols established by the World Allergy Organization, which emphasize symptom progression over binary decision-making.
Additionally, the normalization of stock epinephrine in educational settings raises pharmacovigilance concerns. The FDA has not approved non-prescribed epinephrine for indiscriminate use, and liability exposure for institutions that administer it without a confirmed diagnosis remains significant. This piece reads less like a public health guideline and more like advocacy-driven sensationalism.
Recommendation: Replace emotional appeals with evidence-based clinical algorithms and standardized diagnostic criteria before implementing universal mandates.
Andy Grace
December 27, 2025 AT 15:52Just wanted to say-I’ve been an EMT for 18 years. I’ve seen too many anaphylaxis cases where the delay wasn’t because of ignorance. It was because someone was waiting for permission.
Once, a teenager collapsed at a high school football game. The nurse had the EpiPen. But she called the principal first. By the time they got approval, the kid was in cardiac arrest. He survived. But barely.
Epinephrine isn’t a decision. It’s a reflex. Like pulling a fire alarm. You don’t ask if the smoke is "serious enough." You act.
I’m not a parent. I’m not a teacher. I’m just someone who’s seen the aftermath. Don’t wait for a rulebook. If someone’s turning blue and can’t breathe-give the shot. Then call 911.
And if your workplace doesn’t have a plan? Make one. Today.
Delilah Rose
December 29, 2025 AT 01:31I’ve spent the last five years as a parent of a child with multiple food allergies, and let me tell you-this isn’t about paperwork. It’s about trust. The first time my daughter had a reaction at school, I cried in the parking lot because I didn’t know if the teacher would know what to do. Turns out, she did. Because the school had trained everyone. Even the lunch ladies. Even the bus driver.
But here’s the thing: the plan only works if it’s alive. Not just on a clipboard. Not just in a drawer. It’s alive when the new substitute teacher knows where the EpiPens are. When the kid with the allergy doesn’t have to explain their condition every time they eat lunch. When the principal doesn’t say "we’ll see" when you ask if the plan was updated.
And workplaces? Same thing. My husband works in construction. He’s got a bee sting allergy. Last summer, someone in his crew got stung. No one knew what to do. He had to yell for his EpiPen. He’s fine now. But he won’t let his team go on a job site without a training session. He’s not asking for special treatment. He’s asking to be seen as someone who deserves to come home at night.
So if you’re reading this and you’re in charge-don’t wait for a lawsuit. Don’t wait for a tragedy. Just do the right thing. Because the right thing isn’t complicated. It’s just inconvenient. And inconvenient is better than dead.
Spencer Garcia
December 30, 2025 AT 18:59Epinephrine first. Always. No exceptions. Train two people per location. Store it where the reaction happens-not in the office. Update the plan every year. Done.
Stop overcomplicating it. People die because we make it a debate instead of a protocol.
Abby Polhill
January 1, 2026 AT 16:56From a clinical operations standpoint, the framework outlined here aligns with best-practice guidelines under the FARE-ADA interoperability model, particularly around tiered response protocols and non-prescriptive epinephrine deployment. The integration of digital platforms like FARE’s real-time alert system introduces a critical layer of compliance automation-reducing human error in contact tracing and training verification.
That said, the current adoption curve in workplace settings remains hamstrung by liability misperceptions and siloed HR infrastructure. The ADA’s "reasonable accommodation" clause is often interpreted as a passive obligation rather than an active safety imperative. We need to reframe this as a risk mitigation strategy-not a compliance checkbox.
Pro tip: Pair epinephrine access with QR-coded digital plans. Scan it, read the protocol, hear the voice-guided instructions. No training required. Just action. The FDA’s upcoming voice-enabled devices will be a game-changer for high-turnover environments. If your org isn’t piloting this by Q3 2025, you’re already behind.
Rachel Cericola
January 3, 2026 AT 14:45Let’s cut the fluff. If you’re running a school or a workplace and you don’t have a clear, actionable, trained, accessible anaphylaxis plan-you’re not just negligent. You’re a liability waiting to happen.
I’ve sat in too many meetings where HR says, "We don’t have the budget," or "We don’t have the staff," or "We’ve never had an incident." Guess what? You won’t have one until you do. And then it’ll be too late.
Epinephrine isn’t expensive. Training isn’t time-consuming. A laminated poster and a 20-minute demo? That’s it. But you won’t do it unless someone forces you. So here’s what I’m doing: I’m emailing every school board and HR director I know this post. And I’m tagging them in it. And I’m not stopping until every single one of them has a plan that doesn’t just exist on paper-but lives in the hands of every person who walks through the door.
If you think this is overkill, go read the obituary of the 12-year-old in Texas. Then tell me again that this isn’t urgent.
This isn’t about being nice. It’s about not being a murderer by omission.
Blow Job
January 3, 2026 AT 17:52Just wanted to say-I’ve trained over 200 people on epinephrine use. Mostly in restaurants. Most of them were terrified. "What if I mess up?" they’d say.
I told them: "You won’t mess up. The pen does the work. You just press it. Like a doorbell. It clicks. That’s it.
One guy, a cook, said he’d never use it on a customer. "I’m not a nurse," he said.
I said: "You’re the only person who’ll be there when they collapse. That makes you their nurse right now."
He used it last month on a customer who had a peanut reaction. Saved his life.
People don’t need more rules. They need to know they’re allowed to be the hero. So tell them. Show them. Let them practice.
And if you’re the boss? Make it mandatory. Not optional. Not "if you have time." Mandatory.
Because when it happens, you won’t have time.
Christine Détraz
January 5, 2026 AT 06:28My son’s school has a plan. It’s posted on the wall. Everyone knows where the EpiPens are. The janitor, the librarian, the art teacher-they’ve all done the training.
But here’s what I didn’t expect: my daughter’s classmate with a milk allergy started asking her friends to carry a spare EpiPen in their backpacks. "Just in case," she said.
They did.
It’s not just about rules. It’s about community. When kids learn to look out for each other, the plan becomes something alive.
Workplaces could learn from that.
Maybe we don’t need more policies.
Maybe we just need more people who care enough to act.